Inconceivable?
May 1, 2022 Return

Knowing the possible causes of infertility would help you gain a better understanding of fertility treatments, which in turn would give you a boost of confidence to keep on trying even when you encounter some stumbling blocks along the way. So, let’s take a look at some of these causes.
It’s not always better late than never
Dr Wong Pak Seng points out that people today are having children at a later age, for reasons such as focusing on their careers or wishing to achieve financial stability first. However, the fertility of a woman decreases with age.
Source: Management of the Infertile Woman by Helen A Carcio and The Fertility Sourcebook by M Sara Rosenthal
As can be seen from the chart, a woman’s chances of becoming pregnant begin to decrease sharply after she turns 40.
This decrease in fertility could be due to the fact that the number of good quality eggs produced by the ovaries naturally declines with age.
“At birth, the ovaries contain about 1 million eggs. This number falls to about 400,000 during puberty, and keeps falling with age,” explains Dr Wong. “This is why a 40-year old woman may find it harder to conceive compared to a 30-year old woman.”
This is not to say that a woman over 40 will certainly have difficulties in getting pregnant, of course. A successful pregnancy is not merely biology in motion – a little luck may be involved too, sometimes. But in principle, with declining fertility, there is a higher chance that a woman over 40 may take longer or require fertility treatment to become pregnant. Dr Wong notes that a significant number of his patients are older women.
Having said that, younger women – and their husbands – may also require fertility treatment, as problems in conceiving are not solely due to age and decreased fertility.
A problem with biology
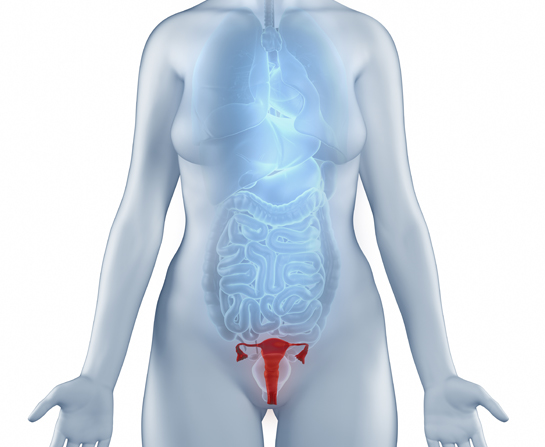
Problems in the reproductive system could be the reason behind a couple’s inability to conceive. But before we go into these reasons, let’s rediscover how the reproductive system works.
To understand the process behind the creation of new life, let’s take a look at the ovaries first. In the woman’s ovaries, there are a large number of eggs, but only one will win the biological lottery and matures into an ovum. The ovum is released by the ovary around the 9th day of the menstrual cycle into the tunnel-like structure called the fallopian tube, which connects the ovary to the uterus.
If sexual intercourse were to take place around this period, about anything from 40 to 60 million sperm would be ejaculated into the womb, during which most would die immediately. Those that survive swim in the fluids of the uterus, looking for the elusive ovum. The one sperm that reaches the ovum would fuse with it in a process called fertilisation, contributing its genetic material and triggering subsequent development of the fertilised egg.
The fertilised egg continues to travel to the uterus until it implants itself into the thickened wall of the endometrium (the inner wall of the uterus). This occurs within 6 days after fertilisation. Through a series of interactions with hormones, the endometrium has undergone thickening and structural changes to accommodate the implantation. Once the fertilised egg is well-implanted, it continues to develop into a foetus and, eventually, a fully formed baby is ready to enter this world.
With the exception of fertilisation, the entire process from the development of eggs to the implantation is tightly controlled by the hormones. If you consider the body a well-oiled factory, there are various body parts that monitor the progress and, when action is needed to start, accelerate, slow or stop a process, these body parts will release hormones which act as “workers” to effect the required changes. Here are just some of the many “workers” involved in the reproductive process.
| Hormone | What it does |
|---|---|
| Follicular stimulating hormone (FSH) | High levels trigger the development of egg cells in women and sperm cells in men. |
| Luteinising hormone (LH) | In men, it helps regulate the production of testosterone (see below). In women, it helps regulate the menstrual cycle and egg production. |
| Hormone | What it does |
|---|---|
| Human chorionic gonadotropin (HCG) | Produced by the structure that eventually becomes the placenta, it tells the body that a pregnancy is taking place, so it is time to stop creating new ovum, halt the menstruation cycle and prepare the body to nurture the new life growing inside it. High levels of HCG are to be blamed for morning sickness, so this is definitely a “hate it, but can’t live without it” type of hormone! |
| Progesterone | This hormone keeps the uterus muscle relaxed in order for implantation to take place, and alerts the body to keep the environment within the uterus to remain within healthy limits for the foetus to develop. We will discuss more about this hormone later. |
| Oestrogen | This hormone plays a key role in the development of the foetus. |
| Hormone | What it does |
|---|---|
| Testosterone | Plays a role in sperm development |
Hormones do not act alone; they often interact with other hormones, either to support or counter the effect of those other hormones. For example:
- High levels of GnRH triggers increased release of LH.
- After LH level reaches a certain amount, the ovaries respond by releasing a mature egg into the fallopian tube.
- The follicle from which the mature egg came reacts to the elevated of LH by producing and releasing progesterone.
- Progesterone causes the endometrium to prepare for implantation and stops production of any subsequent mature eggs.
- If a pregnancy does not occur, high levels of progesterone trigger a decrease in the amount of GnRH released. Decreasing GnRH levels in turn triggers a decrease in LH level, and this in turn inhibits further progesterone secretion.
- The above does not happen when pregnancy occurs. Instead, progesterone level remains high to ensure that pregnancy is maintained during the delivery date.
As you can see, a successful pregnancy is not solely about ensuring a successful fertilisation of an ovum by a sperm. Thus, any breakdown in this complex process can prevent a successful pregnancy. Perhaps there are not enough hormones to trigger production of enough sperm, eggs, or both. Perhaps implantation cannot take place because of the lack of relevant hormones or there are physical abnormalities that prevent the process from taking place.
Diseases and health conditions that affect the womb may also cause damage that interfere or disrupt a successful pregnancy.
As an example, Dr Wong brings up endometriosis. This is a condition in which tissues from the endometrium end up growing in places such as the fallopian tubes and the ovaries. This long-term condition can cause scars, lesions and even cysts to develop in those places, all of which can affect one’s ability to conceive.
“There are many possible reasons, which could only be determined after a thorough medical examination at the fertility centre,” says Dr Wong.
How is your life?
Lifestyle choices can affect fertility. Smoking is an example of a habit that could reduce fertility, according to Dr Wong. This is because the chemicals present in tobacco can damage sperm cells. As the effect can occur even when the man only inhales cigarette fumes, many fertility specialists encourage a couple to stop the habit, even if it is the wife, not the husband, who is the smoker.

What you consume and how much exercise you do each day can affect your fertility as well, since they affect your body weight. Overweight and obese people tend to have increased risk of diabetes and other health conditions that can affect fertility. Dr Wong also points out that the use of recreational drugs and excessive alcohol drinking can negatively affect fertility and these habits should be avoided.
Dr Wong adds that should one or both partners have had multiple sexual partners in the past, any sexually transmitted infections (STIs) they contracted can also affect their fertility. For instance, certain STIs such as chlamydia infection can cause pelvic inflammatory disease (PID) in the woman. If left untreated, PID can lead to formation of scar tissue or blockage of the fallopian tubes and subsequent infertility.
Therefore, when the fertility specialist team makes enquiries on your lifestyle and sexual history, it is best to answer honestly, as the more they know about the possible causes of your infertility, the easier it would be for them to devise a suitable treatment programme to help you conceive. They will not judge or reveal your potentially embarrassing answers to anyone – privacy is very important in the relationship between a doctor and his or her patients!
Other forms of health problems
Aside from STIs, there are other types of infections that may affect fertility too. Dr Wong mentions mumps as an example – men who had mumps when they were younger can have lower fertility rate because the virus can cause the testicles to become inflamed (a condition called orchitis) and sperm production to stop.
There are various health conditions that can also negatively affect fertility. A woman with polycystic ovarian syndrome (PCOS), for instance, often has difficulties getting pregnant because her hormonal system is out of balance. She may have too much male sex hormone, for example, and this would hamper egg production in her ovaries.
A complete mystery
Dr Wong points out that it is possible that a fertility specialist team may not be able to discover the exact reasons why a couple is infertile even after thorough testing and examination. It is estimated that 20% of couples undergoing fertility fall under this category.
This is because, as you have seen, the reproductive system is controlled by a very complex series of interactions with hormones and other substances (including those in our food, drinks and the environment), and we are still discovering new things to this day. Therefore, it is possible that a couple’s infertility is caused by something that we have yet to identify.
Fortunately, treatment can still proceed even if the exact cause is unknown. The fertility specialist can fall back on his or her knowledge and experience to devise the most appropriate treatment.
Now, let’s take a look at making that first step to having a baby despite the odds: booking that appointment with a fertility specialist.
References:
Collins J A. (2004). Evidence-based infertility: evaluation of the female partner. International Congress Series; 1266:57-62. Retrieved at 8 April, 2015, from http://www.researchgate.net/publication/248213025_Evidence-based_infertility_evaluation_of_the_female_partner.
Patient.co.uk. The Female Reproductive System. Retrieved at 8 April, 2015, from http://www.patient.co.uk/health/the-female-reproductive-system.
WebMD. Your Guide to the Female Reproductive System. Retrieved at 8 April, 2015, from http://www.webmd.com/sex-relationships/guide/your-guide-female-reproducti
[1] Patient.co.uk. The Female Reproductive System. Retrieved at 8 April, 2015, from http://www.patient.co.uk/health/the-female-reproductive-system.
[2] WebMD. Your Guide to the Female Reproductive System. Retrieved at 8 April, 2015, from http://www.webmd.com/sex-relationships/guide/your-guide-female-reproductive-system
[3] Patient.co.uk. The Female Reproductive System. Retrieved at 8 April, 2015, from http://www.patient.co.uk/health/the-female-reproductive-system.
[4] Collins J A. (2004). Evidence-based infertility: evaluation of the female partner. International Congress Series; 1266:57-62. Available at http://www.researchgate.net/publication/248213025_Evidence-based_infertility_evaluation_of_the_female_partner; accessed 8 April 2015.
If you like this article, do subscribe here.