A Conversation About Nasopharyngeal Carcinoma
April 28, 2022 Return

INTERVIEW LIM TECK CHOON
Dr Johnson Ng Wei Siang ENT/Head & Neck Surgeon |
Nose cancer comes to the forefront of Malaysians’ minds when Datuk Lee Chong Wei revealed that he was diagnosed with this cancer last year.
This month, HealthToday catches up with an ENT/head and neck surgeon to take a closer look into a common nose cancer, nasopharyngeal carcinoma, and how it affects Malaysians, particularly the Chinese community.
HT: It is said that nasopharyngeal carcinoma (NPC) is difficult to detect. Why is that so?
Nasopharyngeal carcinoma is a cancer that arises from the region of the nasopharynx, which is in the upper area of the throat that lies behind the nose and just below the base of skull.
Cancers arising from the region of nasopharynx are difficult to detect for a few known reasons. One is that it arises from a site that is inaccessible and obscured from sight. Secondly,its early growth can be completely asymptomatic, or its early symptoms can be very non-specific and mild that many do not seek medical attention earlier on.
Another major contribution to its usually late detection lies with the lack of awareness of this potentially life-threatening disease among the general public and some of our healthcare providers. The recent unfortunate high-profile event that happened to our national shuttler has seen some sudden spike in awareness as well as change in attitude among the general public on this disease.
CANCERS ARISING FROM THE REGION OF NASOPHARYNX ARE DIFFICULT TO DETECT FOR A FEW KNOWN REASONS.
HT: What are the symptoms of NPC?
The symptoms of NPC can be more easily understood if it’s classified into localised, regional or distant symptoms.
In the earlier phase of cancer growth, it could cause progressive nose block usually on one side, nosebleed or blood stained nasal discharge and sputum. As our ear is connected to our nasopharynx via the Eustachian tube, ear symptoms are also early signs of potential disease. Similar to having ear symptoms such as ear pain, ear block sensation, reduced hearing and ringing sound in the ear during a bout of bad flu, a growing tumour in the region of nasopharynx will also produce similar symptoms.
As the tumour grows further, it will erode and invade its nearby structures. It can extend forward into the orbit (eye) or upwards into the base of skull to involve the important cranial nerves in our head and neck region. These nerves control movements of our eye, sensation on our face, movements of our vocal folds, tongue etc.
The region of the nasopharynx is also rich in lymphatic drainage. Hence, it is very common that regional presentation with a neck swelling is commonly the earliest symptoms that many patients seek medical attention for prior to diagnosis. Our body lymphatic system works like a filter against infection or cancer cells. Unlike infection where the lymph node swelling is usually painful and resolves after the infection settles, cancer in the lymph node is usually painless and progressively increases in size over time.
Distant symptoms of NPC are late symptoms of disease due to the cancer spread elsewhere in the body including the brain, lungs, liver and bone. Seizures, difficulty breathing, jaundice, and bone pain are some of such symptoms.
Finally, there are also generalised symptoms of any cancer including significant unexplained weight loss and loss of appetite.
HT: What is the prevalence and incidence of NPC in Malaysia? At what age is NPC commonly detected?
The prevalence of NPC varies worldwide. It is a predominant disease especially among the ethnic Chinese. Globally its incidence is only less than 1-in-100,000. However, in endemic areas including some parts of Southern China and Hong Kong, its incidence rises to over 20 per 100,000 population.
In Malaysia, according to the Ministry of Health Cancer Registry 2007-2011, NPC is ranked the fifth most common cancer overall in Malaysia accounting for about 5% of all cancers registered. However, it is the third most common cancer among the males coming in only after colorectal and lung cancer with an incidence rate of 6.4-in-100,000 male population. Its calculated lifetime risk for NPC in Malaysia is 1-in-143 for all males and 1-in-417 for all females which translates to male to female ratio of 3:1.
Among the different ethnic groups in Malaysia, NPC is most common among the ethnic Chinese (49%) followed by the natives of Sabah and Sarawak (28%) and Malay (22%). In Sarawak, NPC among Bidayuh accounts for 48.4% of its cases.
The most common age group at presentation is 40-60 years old. However, NPC may occur even in the younger age group where its risk among the male starts increasing from 25 years. The youngest case of NPC was diagnosed at 6 years of age.

HT: What are the possible causes of NPC?
At present, there is no direct genetic mutation that could be linked to NPC. However, we are 3-8 times more likely to develop NPC in our lifetime if we have a positive first-degree relative with NPC.
In terms of lifestyle, smoking and eating salted fish has been shown to be major risk contributors to develop NPC.
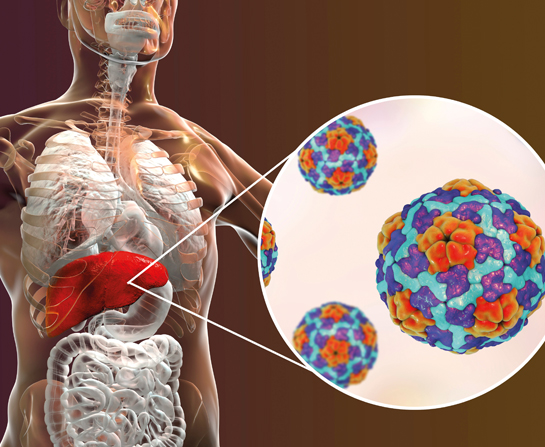
Epstein-Barr virus (EBV) infection has also been strongly linked to NPC. It is a member of the human herpesvirus family and it causes one of the most common human virus infections worldwide. Infection spreads via the saliva of the infected person and the virus persists and remains dormant in the body after infection. Currently, EBV antibodies are used as a screening tool for high-risk individuals for NPC.
HT: What are the standard treatments for NPC?
For newly diagnosed NPC, primary treatment would involve some form of radiotherapy usually in combination with chemotherapy unless the disease is in its very early stages.
The newer generation of radiotherapy, intensity modulated radiotherapy(IMRT), has greatly improved treatment outcomes for NPC while reducing its side effects.
For local recurrent cases (the cancer coming back at or near the same place as the original tumour), advancements in radiotherapy delivery with options of image-guided radiotherapy and CyberKnife® are now available.Surgery excising the nasopharynx (nasopharyngectomy) may also be considered.
For regional recurrence (the tumour has grown into lymph nodes and/or surrounding tissue near the original tumour location) or residual disease in the neck, surgery involving some forms of neck dissection is currently the recommended treatment of choice.
HT: What are the common complications caused by NPC?
As the disease progresses, one of the most debilitating complications arises when the disease invades the base of skull to involve the important cranial nerves in the head and neck region. It can cause blindness, affect the eye movement causing a squint and double vision, numbness over the face, voice change, choking episodes and difficulty swallowing. It can also cause intense headache from the raised pressure within the skull vault.
Distant spread to brain, lungs and bone can cause seizures, difficulty breathing and intense back pain. NPC like any other cancers can be life threatening if not detected early.
Complications from treatment process are due to the side effects of the radiotherapy and chemotherapy. Radiotherapy side effects include excessive dry mouth, oral ulcers, dental caries, osteoradionecrosis and skin burns while chemotherapy can cause toxicity to the ears, heart or kidneys.
PATIENTS WITH NON- RESOLVING NECK SWELLING, EAR OR NASAL SYMPTOMS SHOULD SEEK MEDICAL ATTENTION EARLY SO AS NOT TO MISS AN EARLY CANCER.
HT: At which stage of NPC will patients have the best chances of survival when treated?
The survival of NPC is markedly improved in the early stages of disease. Cancer outcome is usually measured based on overall 5-year survival.
In stage 1 disease, the 5-year survival is about 90%. Although its outcome is only measured up to 5 years, many patients do remain cured and survive many years beyond. For stage 2 and 3 disease, the 5-year survival drops to 60-70% while for stage IV disease it is less than 40% without distant spread and 0% with distant spread.
Unfortunately, only 10% of cases present with stage 1 disease while over 60% presenting in the later stages of stage 3 and 4 disease. The lack of awareness among the general public and some healthcare providers remain the main stumbling block that prevents early diagnosis of the disease. Patients with non-resolving neck swelling, ear or nasal symptoms should seek medical attention early so as not to miss an early cancer. HT
If you like this article, do subscribe here.