Thinking about getting your wisdom tooth removed? Oral surgeon Dr Andrew Chan Kieng Hock explains why not all wisdom teeth need to go, what the surgery involves, and how to avoid the worst of the post-op misery. Here’s what you need to know before that dental chair reclines.
WORDS DR ANDREW CHAN KIENG HOCK
 FEATURED EXPERT FEATURED EXPERTDR ANDREW CHAN KIENG HOCK Dental Surgeon Klinik Pergigian Ooi Dan Rakan |
Wisdom tooth removal is one of the most common minor surgeries performed in dental clinics, usually under local anaesthesia.
But when things get complicated, it’s best handled by a trained oral or maxillofacial surgeon to minimize discomfort and reduce the risk of complications.
UNDERSTANDING WISDOM TEETH
- Wisdom teeth, or third molars, usually show up between the ages of 18 and 25, although some people get them later.
- Because they’re the last adult teeth to emerge, they often run out of room in the gums.
- This can cause pain, swelling, or even fever during tooth eruption.
When a Wisdom Tooth is Impacted
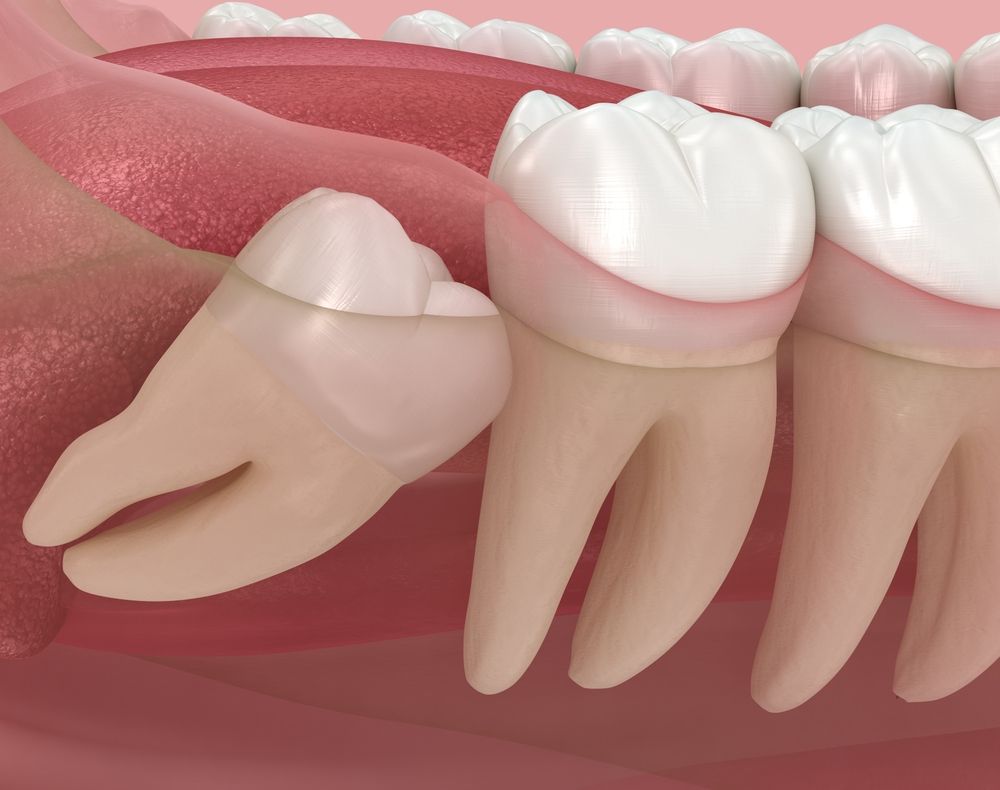
An “impacted” wisdom tooth is one that hasn’t fully emerged into its proper chewing position.
- This can happen because there is not enough space, it is blocked by another tooth, or it is developing at an odd angle.
- Sometimes, a tooth is even fused to the jawbone, although that is a rare occurrence.
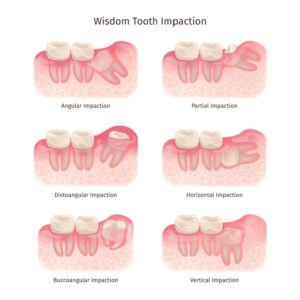
Impaction can be:
- Complete. Entirely buried under the gum or bone, and invisible.
- Partial. Partially visible but not in the right position to function.
Studies show that 25% to 73% of adults have at least one impacted wisdom tooth.
- The wide range is due to different approaches among dentists.
- Some recommend removing wisdom teeth even if they are not causing problems, while others prefer a wait-and-see approach.
- To guide best practice, dental bodies like the UK’s National Institute for Health and Care Excellence (NICE) have published clinical guidelines.
WHEN SHOULD A WISDOM TOOTH BE REMOVED?
Not every impacted wisdom tooth needs surgery.
- The decision should be based on a careful evaluation of risks versus benefits.
- If a tooth is likely to cause problems, removal is reasonable.
- If it is healthy and not causing issues, keeping it may be the better option.
Common Reasons to Remove a Wisdom Tooth
Medical issues
- Severe tooth decay that cannot be treated, especially when it affects nearby teeth.
- Untreatable infection inside or around the tooth.
- Recurring gum infections (pericoronitis), especially after the second episode or a particularly severe first one. Sometimes just removing the gum flap helps, but the problem can come back.
- More serious infections, like cellulitis (widespread tissue infection), abscesses (pockets of pus), or bone infections (osteomyelitis).
- Medical conditions that increase the risk of infection, such as heart valve problems, organ transplants, joint implants, chemotherapy, or radiotherapy.
- Tooth damage, including internal or external breakdown of the wisdom tooth or nearby teeth.
- Fractured teeth or teeth in the line of a jaw fracture.
- Cyst or tumour development, such as dentigerous cysts or ameloblastomas.
Obstruction issues
- Orthodontic reasons, such as making space for braces. However, there’s little evidence that removing wisdom teeth prevents future crowding.
- Obstruction to other dental work, like dentures or tooth restorations.
- Surgical planning, where the tooth blocks jaw reconstruction or lies in a radiation field.
Tooth donation
- In rare cases where a wisdom tooth is used for intentional transplantation.
Other reasons
- Sometimes, removal is considered for practical reasons, such as for people working in remote locations (military, oil rigs, etc) where access to emergency dental care can be limited.
If none of these reasons apply, and the wisdom tooth is not causing issues, regular check-ups every 6 to 12 months are important to monitor any changes.
WHAT ABOUT THE OPPOSING TOOTH?
If a problem tooth is removed, the one directly opposite it (the “contralateral” tooth) may also need to be taken out, especially if it causes issues like biting into the gum.
WHAT TO EXPECT DURING WISDOM TOOTH REMOVAL
In straightforward cases, wisdom tooth removal is a minor outpatient procedure with minimal risks.
Before the Surgery
Your dental surgeon will review your medical and dental history, perform an exam, and take X-rays to map the tooth’s position and its relationship to important structures like the lower jaw nerve.
Anaesthesia Options
- Local anaesthesia, most common in clinics.
- Intravenous (IV) sedation, sometimes added for extra comfort.
- General anaesthesia, used in hospitals for complex cases or when removing all four wisdom teeth at once.
After the Surgery
You will be given painkillers, antibiotics, and anti-inflammatory medication.
Good oral hygiene and following your dentist’s instructions will help ensure a smooth recovery.
COMPLICATIONS?
It is normal to have swelling, pain, and a limited ability to open your mouth for a few days. Most people recover within a week.
Possible but uncommon complications include:
- Excessive bleeding or swelling
- Prolonged pain
- Dry socket (pain from dislodged blood clot)
- Severe lockjaw (trismus)
- Infections
- Osteomyelitis (bone infection)
- Nerve injury, causing numbness or tingling (usually temporary, rarely permanent)
- Jaw fracture
- Sinus complications, like an opening between mouth and sinus cavity (oroantral fistula)
IN CONCLUSION
- Deciding whether to remove a wisdom tooth isn’t always straightforward, even for dentists.
- Every case is different, and what works for one person may not be right for another.
- A good surgeon will assess each patient carefully and weigh all the risks and benefits before proceeding.
- There’s no one-size-fits-all approach — just good judgment and clear communication.
| This article is part of our series on health issues and advice related to oral health. |