The Sweetest Sorrows: To Keep the Light in Your Eyes
April 29, 2022 Return
Dr Nor Fariza binti Ngah Head of Department, Department of Ophthalmology, Hospital Shah Alam
In addition to the heart, type 2 diabetes can also affect the eyes. “For many people with diabetes, it is not a matter of if, but rather, when they develop diabetic eye disease,” says Dr Hjh Nor Fariza binti Ngah, an ophthalmologist who is also the Head of the Department of Ophthalmology in Hospital Shah Alam.
But before we look at these diseases, let’s first take a look at how diabetes affects the eye.
A closer look at the eyes
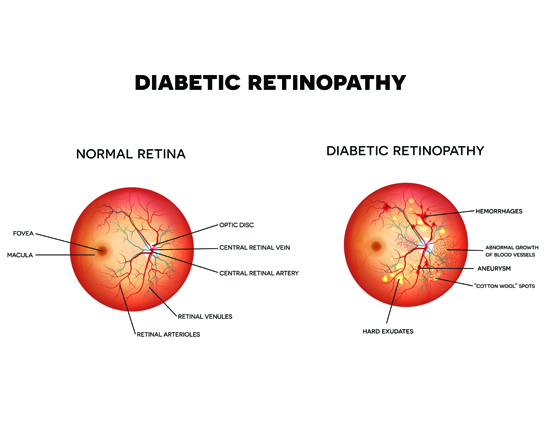
The front of your eyes contains the cornea and the lens. When you look at something, light passes through the cornea and then the lens. These two structures acts to focus the light, so that it will be directed to the innermost layer of the eye called the retina. It is at the retina that light-sensitive cells convert the light into electrical signals, sent through the eye nerves to the brain, which then read these signals and tell you what you are seeing. When light is focused on a tiny region called the macula, you will see things in more detail (making out of alphabets during reading, telling apart different colours on a painting, etc). Other regions of the retina are responsible for transmitting signals for peripheral or side vision.
The retina is nourished by a network of fine blood vessels, which supply oxygen and nutrients to ensure that its cells can function at tip-top condition. In people with diabetes, these blood vessels are vulnerable to high blood glucose levels, especially when the diabetes is poorly controlled. Damage to these blood vessels will give rise to one of the most serious diabetic eye disease: diabetic retinopathy.
Diabetic retinopathy
According to Dr Nor Fariza, diabetes can cause the fine blood vessels in the retina to either become blocked or leak into surrounding tissue, and this can affect the person’s vision. Because diabetes can slow down wound healing, the body has a harder time repairing these leaks and blockages. This situation is also complicated by diabetes which makes the eye drier than normal. Further complications can arise from the presence of microorganisms that can cause infections.
Diabetic retinopathy does not show any early symptoms, so Dr Nor Fariza rightfully considers it a ‘silent’ threat to people with diabetes.
“People with diabetes will get diabetic retinopathy,” says Dr Nor Fariza. “But for people with good diabetes control, this condition can be very mild – perhaps just one small dot-like area of haemorrhage.”
During the early stage
- Very mild effects are seen on the blood vessels. There are some slight bulging (microaneurysm) and leakages of blood or other fluids.
- As long as the region containing the macula is still unaffected, you will be able to see normally. Hence, you will not likely be aware that you have this condition unless you get your eyes screened.
- There is always the risk of the condition progressing further until it affects the macula (giving rise to diabetic maculopathy, see below) and hence your vision, so Dr Nor Fariza advises all people with diabetes to go for eye screening once a year since the time they were diagnosed. “Not every doctor is aware of the importance of eye screening, so if your doctor doesn’t bring it up, you should still ask about it,” she further advises.
On eye screening
People with diabetes require specialized eye screening, Dr Nor Fariza points out. This screening is different from the ones typically offered at spectacle shops. “Some shops do have the equipment and the training,” she says, “but not all of them.” Therefore, it is better to visit an ophthalmologist directly for your yearly eye screening.
At more advanced stages
- The blood vessels in the retina become blocked, causing the cells in surrounding areas to die from a lack of oxygen (ischaemia).
- Your eyes will try to grow new blood vessels to meet the demand for oxygen, but things may not turn out as planned.
- These new blood vessels may end up at the wrong places, such as at the surface of the retina and even protruding into the gel-like substance (vitreous gel) that fills the eyeball cavity. They are also pretty weak and can rupture or leak easily.
- As a result, large areas of haemorrhage may occur all over the surface of the eye, causing your vision to be obscured.
- Sometimes, all this spilled blood can be absorbed back and the vision may improve. Some people may experience frequent haemorrhages in the eye, however, and the blood may not be fully absorbed, possibly resulting in permanent blindness.
- Frequent haemorrhages may also cause the formation of scars at the affected area. This can distort the structure of the retina, possibly even causing it to be detached from the rest of the eye to cause significant sight impairment.
But what are your risks?
If you have read this far, you may feel that things are going to be bleak and hopeless where your eyes are concerned. Don’t worry, as Dr Nor Fariza points out that there are ways to minimize your risk of developing diabetic eye diseases. Let’s take a look at what these risks are.
Risk factors that you cannot control
- How long have you had diabetes. The risk goes up the longer you have diabetes.
- Your age. The older you are, the higher is your risk.
But just because you cannot control these risk factors does not mean you have to lose hope. “Get your eyes screened every year,” repeats Dr Nor Fariza – and this is an advice worth repeating, as early detection of diabetic eye diseases make it easier to treat or manage these conditions.
Also, addressing the risk factors that you can control will help improve your odds considerably.
Risk factors under your control
- Your blood glucose level. Count your carbohydrates, eat balanced meals in the right portion sizes and take your medications as advised by your doctor.
- Your blood pressure. If you have high blood pressure, take your medications as advised by the doctor. Don’t overload your meals with unhealthy fats and salt.
- Your cholesterol level. Watch your diet and take your medications.
- Be physically active every day, even if you are not overweight. This helps to control your blood glucose and cholesterol levels as well as your blood pressure. Spend at least 30 minutes a day being active. You can ask your healthcare team for suggestions on appropriate exercises you can take up.
- Stop bad habits such as smoking and drinking alcohol. The risk especially increases should you smoke.
Go for annual eye screening
Wait, you may be thinking, haven’t this been said two times already? Well, this is such an important advice that is still not put into practice by many people, so Dr Nor Fariza has no qualms bringing it up again for the third time. Third time is the charm, after all!
When it comes to glaucoma, cataract and other more obvious eye diseases, Dr Nor Fariza says that patients will go right away to see specialists such as herself, so those problems are often treated in time. What she is more concerned about is the ‘silent’ yet serious diabetic retinopathy.
“Just because your eyesight is fine at the moment, does not mean that everything is in good condition,” she explains. “Diabetic retinopathy has no early symptoms. The only way to detect it at its early stage and take measures to slow its progression is by going for eye screening once a year.”
Research has shown that when diabetic retinopathy is identified early, through retinal screening, and appropriate treatment is given to the patient, there is a 90% reduction in risk of severe vision loss and blindness. Therefore, if you have diabetes and have yet to get your eyes screened, let’s consult an ophthalmologist as soon as possible!
Treating diabetic retinopathy
There are several ways to treat diabetic retinopathy, depending on how advanced the condition is.
At the early stage
For early stages of diabetic retinopathy, Dr Nor Fariza points out that fenofibrate, the medication which is also prescribed to lower the levels of fat in patients with diabetes, can be useful for slowing down the advances of the condition.
“Fenofibrate has been used for quite a while now to treat patients with high cholesterol level,” she explains. “That it can now be also used to treat early stage diabetic retinopathy is still a new thing in Malaysia.” She adds that it will soon catch on, as more awareness spreads among members of the medical community as well as the public.
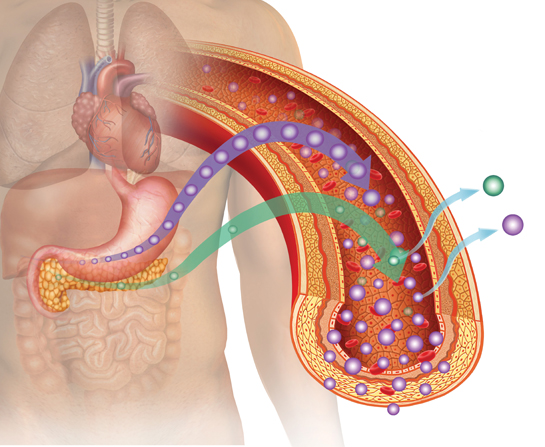
As fenofibrate is taken orally, the obvious benefit is that it will not affect the retina, under laser treatment. As the study below shows, it can also reduce the need for patients to go for laser treatment in the future.
Just how effective is fenofibrate?
Well, the Fenofibrate Intervention and Event Lowering in Diabetes (FIELD) study found that:
- Fenofibrate reduces the need for laser treatment, the first-line treatment for more advanced stage of diabetic retinopathy, in patients with type 2 diabetes.
- For patients with diabetic retinopathy who were given this medication, there was a 31% relative reduction in the need for first laser treatment.
- There was a 79% reduction in the progression of the disease in patients with pre-existing mild to moderate diabetic retinopathy.
At more advanced stages
When diabetic retinopathy reaches a stage where it affects the eyesight, it can be treated using laser treatment when it is detected early enough. Dr Nor Fariza takes the opportunity to remind you again, “This is why you need to go for yearly screening!”
- Laser treatment for the eyes is not the same as laser eye surgery. Laser eye surgery involves the cornea, and serves to improve vision. Laser treatment for diabetic retinopathy will not improve vision; it serves to stop your vision from becoming worse instead.
- For individual or groups of leaking blood vessels, the laser treatment can stop the bleeding and seal these blood vessels. The treatment also helps to reduce any swelling in the retina. This treatment, called a localized laser treatment, is usually quick, taking only a few minutes. Because only a small area of the retina is affected by this treatment, there is usually minimal impact on your vision.
- If the growth of new blood vessels is detected, more extensive laser treatment is needed. This treatment, called the pan-retinal laser treatment, covers a larger area of the retina. After a successful treatment, these new blood vessels will shrink and eventually disappear after a few months. This treatment may affect your vision significantly – there have been reports of patients permanently losing some peripheral vision (which can affect the ability to drive) as well as night and colour vision.
- You may need more than one laser treatment to address your problems.
Dr Nor Fariza says that laser treatment is still the ‘gold standard’ for cases of diabetic retinopathy that have advanced to a stage that threatens the patient’s sight. This is because it is often a permanent, effective way to ensure that the patient’s eyesight will not become worse over time.
- Is it painful? Some discomfort may be experienced, especially for pan-retinal laser treatment. There are ways to relieve the pain, so tell the doctor if you experience pain during the treatment.
- Complications? There are some potential complications, such as reduced night or peripheral (side) vision, which may prevent some people from driving. However, the benefits of getting the laser treatment are generally considered to be greater than the risks of complications.
- Anti-VEGF medications. Aside from laser therapy, there is also the option of injecting a type of medication called the anti-vascular endothelial growth factor (anti-VEGF) directly into the eyes to shrink current blood vessels and prevent the formation of new blood vessels. Some commonly prescribed anti-VEGF medications are ranibizumab and aflibercept.
“Anti-VEGF medications are often an option when laser treatment does not show desired improvements after a few sessions,” says Dr Nor Fariza.
There is another catch: unlike laser therapy, their effects are not permanent; you will have to receive regular injections every few weeks.
Anti-VEGF medications may cause side effects to the heart and blood pressure, possibly leading to a heart attack or stroke. The risks are quite small, but because they exist, these medications are not appropriate for patients who also have hypertension and heart problems.
People with diabetes also face higher risk of developing other eye diseases, such as cataract and glaucoma, all of which could also impair your eyesight and even cause blindness. If you go for yearly eye screening, early stage development of these diseases can also be detected. And just like diabetic retinopathy, good control of diabetes can help reduce your risk of developing these diseases.
Reference:
Noonan, J.E., et al. (2013). An update on the molecular actions of fenofibrate and its clinical effects on diabetic retinopathy and other microvascular end points in patients with diabetes. Diabetes;62(12):3968-75. doi: 10.2337/db13-0800.
If you like this article, do subscribe here.