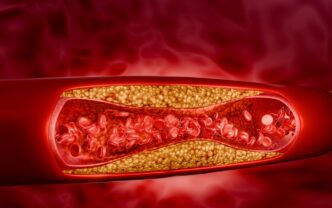
Our arteries are like highways for our blood, carrying oxygen and nutrients to every part of the body. But just like traffic can slow down when roads get clogged, our arteries can also become blocked over time. This happens due to a condition called atherosclerosis, where fatty deposits — made up of cholesterol, cellular waste products, calcium, and fibrin — build up inside the artery walls. As these deposits harden and narrow the arteries, they reduce blood flow, increasing the risk of serious health problems like heart attacks and strokes.
WORDS DR EMMA YAAKOP
 FEATURED EXPERT FEATURED EXPERTDR EMMA YAAKOP Consultant Interventional Cardiologist and Electrophysiologist Columbia Asia Hospital – Puchong |
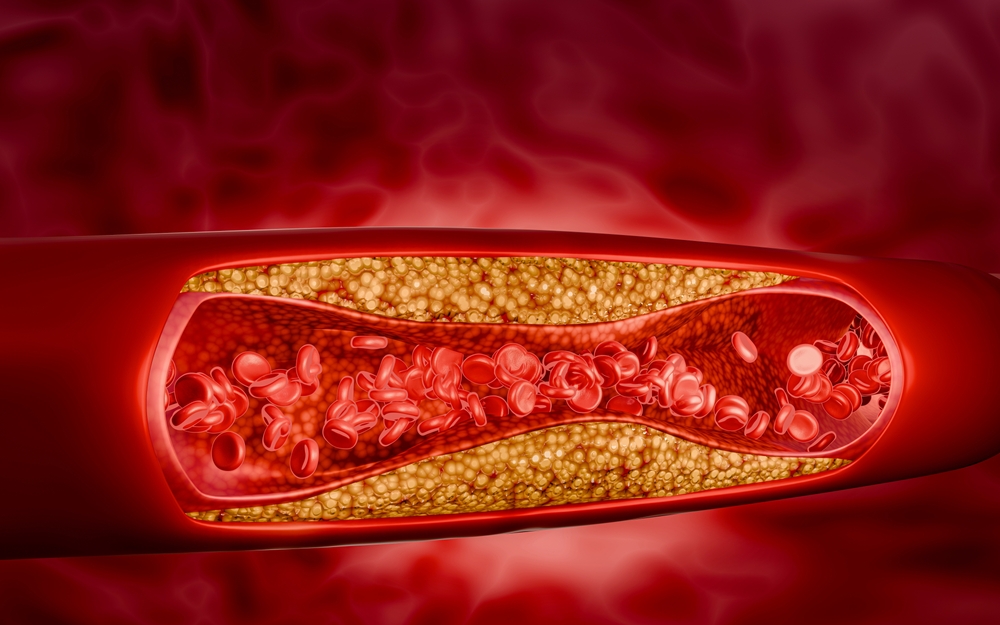
Atherosclerosis doesn’t happen overnight.
- It can begin as early as childhood and this condition may rapidly progress especially in someone with multiple risk factors.
- Studies even show that teenagers can have early signs of plaque buildup, and a generally healthy 40-year-old has a 50% chance of developing serious cardiovascular disease in their lifetime.
- The risk increases with age, and most adults over 60 are affected, often without noticeable symptoms.
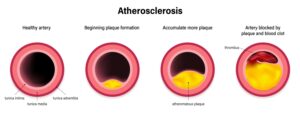
- The atherosclerotic plaque creates a bump on the artery wall through a gradual process that goes on throughout the entire body.
- The plaques may grow to a certain size and stabilize without causing immediate symptoms until middle-age or later.
COMMON RISK FACTORS
The common risk factors behind more than 90% of all heart attacks are:
- Abdominal obesity
- Diabetes and insulin resistance
- Family history of heart disease
- Excessive alcohol intake (more than 1 to 2 drinks per day, depending on body size)
- High blood pressure
- High low-density lipoprotein (LDL) cholesterol
- High triglycerides
- High levels of C-reactive protein (CRP) in the blood, which is a signal of inflammation
- An unhealthy lifestyle such as a poor diet low in fruits and vegetables
- A sedentary routine with little to no exercise
- Smoking
- Chronic or long-term stress
- Sleep apnoea
| For more information on sleep apnoea, click here for Associate Professor Dr Hardip Singh Gendeh’s insight into the topic. |
COMMON POSSIBLE SYMPTOMS
Symptoms from this disease depend on which artery is narrowed or blocked.
For atherosclerosis in the heart arteries:
- Unusual heartbeat, suggestive of cardiac arrhythmia (irregular heart rhythm)
- Pain or pressure in the upper body, including the chest, arms, neck, or jaw (angina)
- Shortness of breath.
For atherosclerosis in the arteries to the brain:
- Numbness or weakness in the arms or legs
- Drooping facial muscles
- Paralysis
- Severe headache
For atherosclerosis in the leg arteries:
- Leg pain when walking (intermittent claudication)
- Numbness
- Cold feet
- Aching or burning in toes and feet while at rest
DIAGNOSING ATHEROSCLEROSIS
Preliminary Checks
- Physical examination by the doctor to checking for weak or absent pulses.
- Blood tests for cholesterol, blood sugar, and other basic risk markers.
- Electrocardiogram (ECG) to record the heart’s electrical activity to detect strain or past damage.
- Chest X-ray to look at heart size and lung changes.
If initial tests show evidence of atherosclerosis, the patient may be referred to cardiologists, neurologists, or vascular specialists for further evaluation and management.
Subsequent/Non-Invasive Imaging
- Echocardiogram, or ultrasound of the heart’s chambers and valves to assess pumping function.
- Exercise stress test (treadmill) to monitor heart rate, blood pressure, and breathing during exertion.
- CT scan or magnetic resonance angiography (MRA) to spot hardened or narrowed arteries.
- Carotid ultrasound to detects plaque in neck arteries.
- Abdominal ultrasound to checks the aorta for bulges or plaque.
- Doppler ultrasound to measures blood flow in arteries.
- Ankle-brachial index, which compares blood pressure in the arms and legs to detect poor circulation.
Invasive/Definitive Tests
- Coronary angiogram, where dye is injected into the arteries and X-rays are then taken to pinpoint the location of the blockages.
WHY ATHEROSCELROSIS NEEDS TO BE TREATED
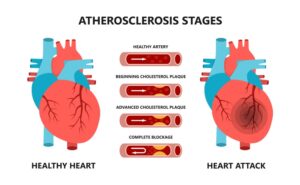
Atherosclerotic plaque disease can lead to 3 main complications of cardiovascular disease.
Coronary artery disease
- The most crucial complication, where stable plaques in the heart’s arteries can cause angina (chest pain).
- A sudden rupture of the plaque can trigger clot formation, leading to a complete blockage and myocardial infarction (heart attack), which can be fatal.
Cerebrovascular Disease
- Happens when the plaque in the brain’s arteries ruptures.
- Such ruptures can cause strokes, potentially leading to permanent brain damage.
- Transient ischemic attacks (TIAs) are early warning signs of a stroke that do not cause lasting injury.
Peripheral Artery Disease
- Due to narrowed leg arteries.
- Causes pain while walking and poor wound healing.
- Potentially lead to limb amputation in severe cases.
TREATMENTS
Atherosclerosis is difficult to reverse.
However, aggressive medical therapy and lifestyle modifications can slow or stop its progression.
Medications
- Medications for high cholesterol, diabetes, and high blood pressure will also reduce the risk of heart attack and stroke.
- This includes blood thinner medication or antiplatelet agents like aspirin, which may help to prevent clot development.
Advanced Treatment Methods
These include:
- Coronary angiography and stenting, where the doctor puts a thin tube into an artery in the arm or leg to get to diseased arteries through a live X-ray.
- Carotid stenting for higher-risk patients to prevent stroke.
- Angioplasty, using a catheter with a balloon tip and stenting to treat blocked arteries.
| Interested to find out more? |
Surgery
- Coronary bypass surgery — a healthy blood vessel is grafted to bypass the blocked artery, restoring blood flow.
- Carotid endarterectomy — plaque in the neck arteries is removed to restore blood flow.
Lifestyle Changes
Therapeutic lifestyle changes help to prevent atherosclerosis or slow down its progression.
- Stress management through yoga, mindfulness, or deep breathing to help lower blood pressure.
- Quitting smoking and vaping are the most important lifestyle changes to prevent damage to the heart from atherosclerosis. In fact, nicotine narrows blood vessels, forcing the heart to work harder, while chemical ingredients in vapes may cause an increase in heart rate, resulting in cardiac arrhythmias and also high blood pressure.
- A healthy diet rich in low-fat proteins, fish, fruits, vegetables, and whole grains will help to manage weight and lower cholesterol, blood pressure, and blood sugar levels.
- Regular exercise will maintain healthy blood pressure and improve blood flow. It is essential to aim for at least 150 minutes of moderate exercise or 75 minutes of brisk exercise a week.
- Compliance with regular check-ups and medication is mandatory for someone who has underlying medical conditions.
| This article is part of our series on the health issues affecting the heart and blood vessels. |