Patent ductus arteriosus (PDA) is a heart defect that affects babies and sometimes adults, too. Dr Siti Laura, a consultant paediatric cardiothoracic surgeon, explains how a tiny device delivered through a vein can fix this issue without the need for open-heart surgery.
WORDS LIM TECK CHOON
 FEATURED EXPERT FEATURED EXPERTDR SITI LAURA Consultant Paediatric Cardiothoracic Surgeon Pantai Hospital Kuala Lumpur |
Patent ductus arteriosus (PDA) is a type of congenital heart defect, meaning that it is a heart problem that is present at birth.
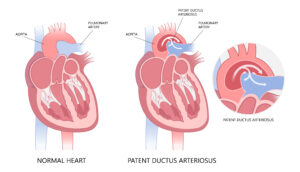
PDA happens when a blood vessel called the ductus arteriosus, which normally closes within 24 hours after birth, stays open.
WHAT HAPPENS WHEN DUCTUS ARTERIOSUS REMAINS OPEN
Dr Siti Laura explains that if left untreated, it can lead to:
- Rapid breathing, shortness of breath, fatigue, and poor weight gain in infants.
- Frequent lung infections.
- Inadequate blood flow to the rest of the body in premature babies, which may cause serious gut problems like necrotizing enterocolitis, an intestinal disease that leads to poor feeding, bloating, blood in stool, and bowel perforations.
- Pulmonary over-circulation, where too much blood flows to the lungs, increasing pressure in the lung vessels (known as pulmonary hypertension) and eventually leading to heart failure.
- A risk of endocarditis (an infection of the heart lining) and thromboembolism (blood clots traveling to other parts of the body).
HOW DOCTORS CLOSE A PDA WITHOUT CLOSE HEART SURGERY
The good news is that many selected cases of PDA can now be treated without the need for close heart surgery.
In selected patients, a procedure called transcatheter device occlusion is the preferred method because it is a minimally invasive, image-guided procedure.
Dr Siti Laura explains how it works:
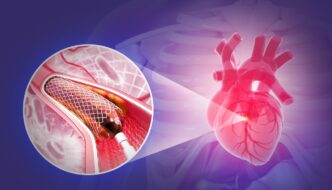
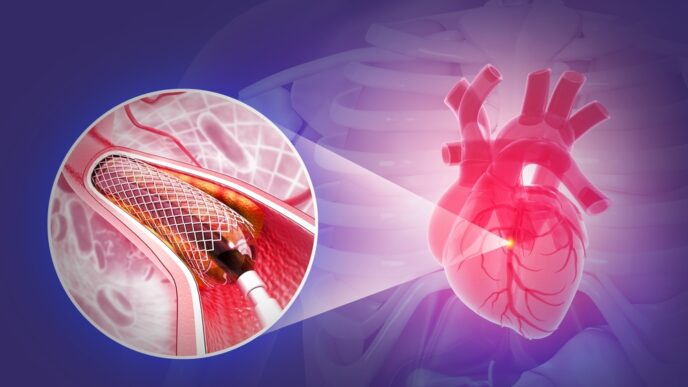
- A small, flexible tube called a catheter is inserted through a vein in the groin area.
- Using a type of live X-ray called fluoroscopy, the surgeon guides the catheter up into the heart and to the PDA.
- A tiny device called PDA occluder, which shaped like a plug or coil, is then delivered through the catheter and placed inside the PDA lumen.

A PDA occluder. Click on the image for a larger and clearer version. - The device expands, anchors itself inside the blood vessel, and blocks abnormal PDA blood flow.
- Over time, the body’s tissue grows around it, sealing the vessel permanently.
Dr Siti Laura adds that this procedure typically takes 1 to 2 hours.
When Transcatheter Device Occlusion Is Not the Best Option
- If one is found to have PDA alongside other heart defects such as a ventricular septal defect (a hole between the heart’s lower chambers) or coarctation of the aorta (a narrowing of the main artery), open surgery may instead be necessary to correct all these issues at once.
- For more complex cases, such as a very large or abnormally shaped PDA, open surgery remains the safer option.
Is There a Difference Between the Procedure When Performed on Small Children to That in Adults?
While the core technique is the same, Dr Siti Laura explains that certain adjustments are made depending on the patient’s age and size.
In infants and small children
- The PDA is often larger relative to their body size.
- Devices and equipment used are specially designed to be smaller and gentler.
In adults
- Their PDA may be hardened by calcium deposits (calcified) or have ballooned out (aneurysmal).
- There is a higher risk of bleeding and perforations in view of the long-standing calcifications.
- Therefore, the PDA occlude device must be carefully chosen to fit the irregular shape of the vessel.
- Adults may also have other medical problems like high blood pressure or diabetes that require extra care.
THE ADVANTAGES OF THIS PROCEDURE
According to Dr Siti Laura, the main benefits of this minimally invasive procedure are:
- No surgical scars on chest, making it cosmetically appealing.
- Shorter hospital stays; usually just 2 to 3 days.
- Faster recovery. Most people can return to their usual activities quickly, though they should avoid heavy lifting, contact sports, or strenuous exercise for a few weeks.
RISKS AND DRAWBACKS TO CONSIDER
Transcatheter device occlusion is generally safe and effective, with high successful closure rates ranging from 94% to 98%.
However, it also carries a low but small potential risk or complication, with a rate of around 2% to 5%.
Risk includes:
- Device migration or embolization. The device might shift from its intended spot, which could block other blood vessels.
- Haemolysis. Red blood cells can become damaged and break down as residual blood flows past a partially closed PDA.
- Narrowing or obstruction of nearby blood vessels, like the aorta or pulmonary arteries.
- Residual shunting. A small leak of blood through the PDA, which often resolves over time.
IN CLOSING: AN ADVICE FROM DR SITI LAURA
For adults who were born with a PDA but never received treatment, Dr Siti Laura has this advice:
Don’t Delay in Seeking Treatment
“Even if you’ve had no major symptoms, untreated PDA can lead to heart failure, pulmonary hypertension, or stroke,” says Dr Siti Laura.
She goes on to advise those affected by PDA to discuss all treatment options with their doctor, including the risks and benefits of each.
Dr Siti Laura also offers the following advice for those that are planning to undergo this procedure:
- Maintain regular check-ups, especially if you have other health conditions.
- Follow activity restrictions as recommended by the doctor, before or after heart procedures.
- To reduce the risk of heart infections (called endocarditis), consider the use of endocarditis prophylaxis during dental or other invasive procedures. Recommendations can vary based on individual situations, so consult your doctor for more information.
- Adopt a heart-healthy lifestyle such as quit smoking, eat well, manage stress, and stay active within safe limits.
| This article is part of our series on the latest developments in the treatment of heart diseases. |