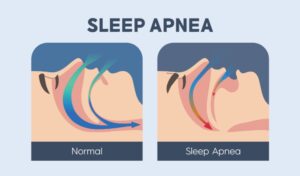
Snoring occurs when the upper airways in the throat region vibrate, resulting in turbulence of air. Snorers are classified into 2 categories; primary snorers or those with obstructive sleep apnoea. Primary snorers often snore and trouble their partners, but it is the second group that we are concerned about.
WORDS ASSOCIATE PROFESSOR DR HARDIP SINGH GENDEH
 FEATURED EXPERT FEATURED EXPERTASSOCIATE PROFESSOR DR HARDIP SINGH GENDEH Lecturer and Specialist Ear, Nose & Throat Surgeon Department of Otorhinolaryngology, Head and Neck Surgery Faculty of Medicine Universiti Kebangsaan Malaysia |
Obstructive sleep apnoea (OSA) is a condition that occurs when there is a stop or cessation of airflow during breathing while one is asleep.
- This results in a decrease in blood oxygen levels.
- As a result, oxygen supply to organs, including the brain, is reduced.
- The brain consequently tries to wake the body up and get it to resume breathing.
- This leads to frequent awakening and disturbed sleep.
Initially the person with OSA may not realize that this phenomenon is occurring to them. It is always the partner in bed beside the person that notices it!
YOU MAY HAVE OSA IF YOU…
- Snore, followed by a short period of silence
- Choke and gasp while asleep
- Frequently wake up from sleep
- Frequently wake up from sleep to urinate (nocturia)
- Feel tired and experience inadequate sleep during daytime
- Experience headaches in the mornings
WHAT CAUSES OSA?
As its name suggests, OSA is caused by any obstruction of the upper airways, such as the pharynx. There are many possible reasons that an obstruction can occur. Here are some of the common ones.
Nose
- Enlarged nasal bones called turbinates.
- Unequal-sized nasal passages due to a deviated nasal septum.
- Inadequate opening of the external nasal passage.
- Enlarged adenoids at the rear of the nose.
- Polyps within the nose.
- Recurrent nasal infections may also be a contributing factor.
Mouth
- Very enlarged tonsils that are almost touching each other.
- A large tongue.
- Soft lower palate.
- Small throat opening.
- Infections/conditions that cause the tongue to be pushed backwards and upwards.
Throat
- Narrowing and collapse of the windpipe.
- Growths within the throat that obstruct the vocal cords and breathing passageways.
Conditions Affecting the Shape of the Head and Face (Craniofacial Abnormalities)
- This is more common among babies and children.
- Certain syndromes will cause a retracted jaw, small face, and/or large tongue, all of which may obstruct airflow while breathing.
- These are often detected at childbirth and managed early.
Obesity
- It is believed that increased in abdominal fat and neck circumferences can lead to the collapse of the side walls of the throat.
WHY OSA CAN BE A SERIOUS PROBLEM
OSA will reduce one’s quality of sleep, often resulting in:
- Sleepiness during the day despite having adequate hours of sleep in the night before
- Fatigue
- Decreased work performance
- Mood changes such as anxiety and depression
- Reduction in sexual performance
- Road traffic accidents or occupational accidents
Prolonged OSA may increase the risk of:
- High blood pressure
- High cholesterol
- Type 2 diabetes
- Increased lung resistance (pulmonary hypertension)
- Heart failure
- Heart attacks
- Stroke
- Premature death.
|
WHAT YOU CAN DO IF YOU BELIEVE THAT YOU HAVE OSA
Step 1: See a General Practitioner
They may ask you to answer a few questionnaires. If your symptoms suggest strongly that you have OSA, a sleep study is next step.
Step 2: Go for a Sleep Study
- Also known as polysomnography, sleep study is considered the gold standard for diagnosing OSA.
- For most cases, a simple sleep test conducted in the comfort of one’s bed or in a normal hospital ward is adequate.
- For a more select group of people, however, the doctor may prescribe a full sleep study at a sleep lab of a hospital, with a sleep technician or doctor present throughout.
|
Step 3: Visit an ENT Specialist
Once OSA is detected, you will be referred to an ear, nose, and throat (ENT) specialist.
They will assess the level of obstruction within your upper breathing passageway, such as by performing a scope of your nose and throat passage while you are under local anaesthesia.
If your OSA is believed to be caused by something other than an obstruction of the upper airways, you will be referred to a neurologist and/or respiratory physician for further assessment.
HOW OSA IS TREATED
The choice of treatment will depend on the severity and level of obstruction that contributes to the OSA.
Continuous Positive Airway Pressure (CPAP) Machine
- This is a device that is used while you are asleep.
- It pumps air into the upper airways and prevents them from narrowing and collapsing while you’re breathing out.
- This helps to prevent interruptions of airflow and allows you to keep breathing while you’re sleeping.
- CPAP machines come in in various models, along with different mask types and sizes.
Surgery
Whether you should be considered for surgery will depend in the levels of airway obstruction, severity and the cause of the obstruction.
The type of surgery considered will depend on the nature and location of the obstruction.
- For example, if your OSA is caused by large tonsils and/or adenoids, then you doctor may recommend the surgical removal of these structures.
- Obstructions in the nose may be addressed through surgical restructuring of the nose and the nostrils opening and/or correction of a bent septum of the nose.
Devices
- Mouth devices to bring forwards a retracted jaw is considered if obstruction is caused by a retracted jaw.
Tracheostomy
- A tracheostomy tube is inserted through the neck, to allow breathing to occur to and from the neck and the lungs, bypassing the nose and mouth.
- This is performed in very severe cases after all other methods have failed to produce desired improvements.
Lifestyle Modification
- Weight loss to achieve a healthier body mass index
- Smoking cessation
- Alcohol avoidance
Sleep Hygiene
Many people tend to overlook the importance of good sleep hygiene.
Good sleep hygiene includes:
- Avoiding caffeine before sleeping
- Sleeping at the same time every day
- Sleeping on a comfortable bed
- Reducing screen time before bedtime
| OSA is often caused by multiple factors, and thus is managed by a multidisciplinary team of healthcare professionals such as general practitioner, ENT specialist, maxillofacial specialist, paediatrician, dietitian, physiotherapist, respiratory physician, etc. If a child has OSA, a paediatrician will also be involved. |
| This article is part of our series on health issues related to the ear, nose, and throat. |















