Immunotherapy has emerged as a promising approach in the war against cancer. Of the available immunotherapy treatments, chimeric antigen receptor (CAR) T-cell immunotherapy in particular has made impressive headways in the treatment of certain cancers such as leukemia and lymphoma.
WORDS AZRI AZERAI
 FEATURED EXPERT FEATURED EXPERTAZRI AZERAI Executive Chairman Malaysian Genomics Resource Centre Berhad |
FIRST, WE’LL NEED TO TALK ABOUT THE T-CELL
The T-cell is a type of white blood cell.
There are 2 types of T-cells.
- Cytotoxic T-cells are the soldier white cells, they kill cells in the body that harbour bacteria and viruses as well as cancer cells.
- Helper T-cells produce signals that are used by other white blood cells, including cytotoxic T-cells, to coordinate attacks on invaders and abnormal cells.
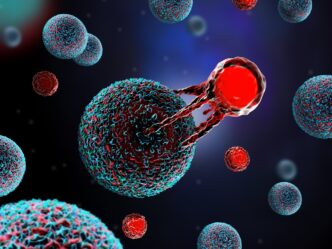
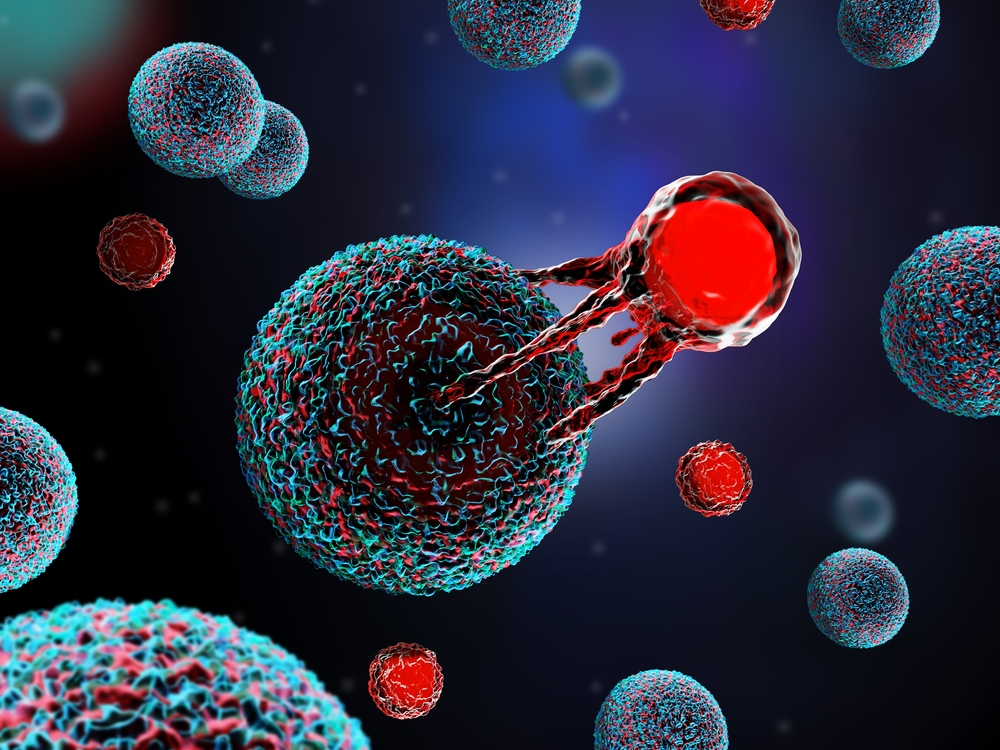
T-cells are generally good at their job, but sometimes, they can have difficulties telling apart normal, healthy cells from cancer cells.
THAT’S WHERE CAR T-CELL IMMUNOTHERAPY COMES IN
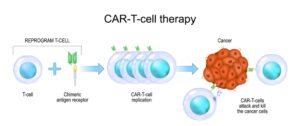
What if we can modify our T-cells to be better at recognizing and killing cancer cells?
That’s what CAR T-cell immunotherapy does.
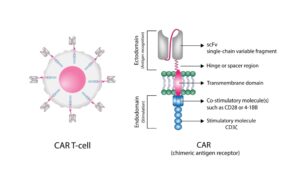
A synthetic structure, called the chimeric antigen receptor (CAR), is attached to the outer layer or membrane of a T-cell — see image above.
The CAR then allows the T-cell to recognize specific proteins on the surface of cancer cells and hence target these cells for destruction — see image above.
THE ADVANTAGES OF CAR T-CELL IMMUNOTHERAPY
- Improves the ability of the patient’s own immune system to eliminate cancer cells.
- CAR T-cells may remain in the body once the patient goes into remission, hence possibly reducing the risk of recurrence to a significant degree.
- Patients may experience a shorter treatment time and reduced side effects compared to many other conventional cancer treatments.
CAR T-CELL IMMUNOTHERAPY WORKS WELL FOR CERTAIN CANCERS
This therapy has been proven to work well for treating cancers of the blood such as leukemia, lymphoma, and multiple myeloma or cancer of the plasma cells.
- The US Food and Drug Administration (FDA) has, in fact, approved 6 types of CAR T-cell products for patients with advanced relapsed or refractory blood cancers.
- Research is ongoing to develop CAR T-cell immunotherapy for solid cancers such as non-small cell lung cancer, kidney cancer, and bone cancer. However, to date none has been approved by the FDA for clinical use.
UNDERGOING CAR-T IMMUNOTHERAPY
Step 1: Assessment
Not everyone with cancer is suitable to undergo CAR T-cell immunotherapy. It works for certain cancers that can be recognized by CAR. Furthermore, the patient needs to be well enough for the treatment.
To determine the patient’s eligibility, the doctor will request a few medical tests for the patient.
The doctor will also take note of the patient’s current health status, history of cancer treatment, and other important details.
Step 2: Collection
Once the patient is found to be eligible, the doctor will collect their blood sample.
Step 3: Extraction
In the laboratory, T-cells are extracted and collected from the blood sample through a process called leukapheresis.
Step 4: Re-engineering
The patient’s collected T-cells are then genetically modified with the introduction of CAR.
The modified T-cells are known as CAR T-cells.
Step 5: Expansion
These CAR T-cells are then cultivated into large numbers in the laboratory.
Step 6: Infusion
Once enough CAR T-cells have been cultivated, they are then transferred back into the patient’s body through an infusion or drip.
These modified T-cells are now better equipped to recognize, target, and destroy cancer cells.
POTENTIAL SIDE EFFECTS
- Cytopenia, or abnormally low levels of red or white blood cells.
- B-cell aphasia. CAR T-cells target selected B-cells of the patient’s own immune system, resulting in weakened immunity against infections. However, this can be treated.
- Cytokine release syndrome, caused by over-activation of T-cells in the body. It is characterized by fever and multiple organ failures.
- Neurotoxicity. CAR T-cells may affect the brain, resulting in headaches, altered consciousness, disorientation, and seizures.
IMPORTANT NOTE
Similar to other cancer treatments, treatment results may vary from one person to another even for the same type of cancer.
If you’re interested in learning more about whether CAR T-cell immunotherapy would be of benefit to you or your loved ones, it’s best to discuss the matter further with a haematologist or an oncologist.
| This article is part of our series on the latest innovations in cancer treatment. |