Imagine waking up to sudden, painless blurriness in one eye. It might feel like nothing serious—but it could be a retinal vein occlusion, often called a “stroke of the eye.” Consultant ophthalmologist Dr Wong Jun Shyan explain what RVO is, who’s at risk, and how early treatment can protect vision and prevent permanent damage.
WORDS LIM TECK CHOON
 FEATURED EXPERT FEATURED EXPERTDR WONG JUN SHYAN Chief Executive Officer ISEC Healthcare |
Retinal vein occlusion occurs when the veins that drain blood from the retina become blocked. Think of it as a “stroke” in the eye.
“There are two main types,” explains Dr Wong Jun Shyan.
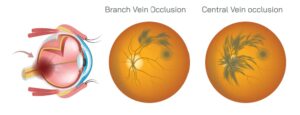
The type of retinal vein occlusion is determined by where the blockage happens in the eye’s veins.
- Branch RVO happens when a smaller vein in the retina gets blocked. This usually affects only a part of the retina, so the damage is more limited.
- Central RVO occurs when the main vein that drains blood from the retina is blocked. This affects the whole retina, making it more serious.
“Even though branch RVO is usually less severe than central RVO, both types can cause vision problems and complications like glaucoma,” says Dr Wong.
“That’s why it’s important to get treatment if needed, no matter which type you have,” he adds.
HOW RVO CAN DEVELOP IN THE EYE
When a retinal vein gets blocked:
- Part of the retina doesn’t get enough blood and oxygen.
- This lack of oxygen can damage the retina.
- The injured retinal cells then release substances called growth factors, such as vascular endothelial growth factor (VEGF), in higher than normal amounts.
- This will cause tiny blood vessels in the retina to leak and the retina to swell, which interferes with its normal function and can lead to vision problems.
What Can Cause the Blockage in the Retinal Vein?
The blockage is caused by a blood clot.
The risk of clot formation increases when one:
- Has high blood pressure or hypertension
- Has diabetes
- Has high cholesterol
- Smokes
- Has increased eye pressure
- Has certain autoimmune conditions
- Uses oral contraceptives
SYMPTOMS OF RVO
RVO often appears to strike without warning, because the early sign are subtle vision changes, such as sudden painless blurring in one eye.
These changes are often easy to miss because the other eye can function well enough to make these changes hard to detect.
DIAGNOSIS OF RVO
- The eye specialist or ophthalmologist detects RVO using a retinal exam.
- The presence of RVO can be confirmed with with imaging tests such as optical coherence tomography (OCT), which checks for macular swelling, or fluorescein angiography, which detects the extent of blockages in the eye.
“Timely treatment greatly influences outcomes,” says the ophthalmologist. “The sooner the swelling is managed, the less permanent is the damage to the retina.”
TREATMENTS FOR RVO
The mainstay of treatment is anti-VEGF injections, which reduce swelling and leakage in the retina.
- “About 80% of patients report vision improvement,” Dr Wong says.
- Mild cases may resolve completely after a few injections.
Severe RVO, however, often requires ongoing therapy to prevent further deterioration to the retina.
- Follow-up therapy involves monthly injections at first.
- The frequency of injections will be gradually spaced out as the retina stabilizes.
- Typically, most patients need 5 to 7 injections in the first year, with subsequent adjustments depending on their response to these initial injections.
Some patients may require retinal laser therapy if the blockages are extensive.
| This article is part of our series on eyesight and eye health. |