Children can be surprisingly good at hiding discomfort, but joint stiffness, fatigue, or a sudden limp may signal something more than growing pains. Paediatric rheumatologist Dr La Reina Sangaran sheds light on juvenile idiopathic arthritis (JIA), its types, early warning signs, treatment advances, and practical advice for families navigating life with this condition.
WORDS DR LA REINA SANGARAN
 FEATURED EXPERT FEATURED EXPERTDR LA REINA SANGARAN Paediatric Rheumatologist Hospital Tuanku Ja’afar |
UNDERSTANDING JUVENILE IDIOPATHIC ARTHRITIS (JIA)
- Juvenile idiopathic arthritis (JIA) is essentially chronic joint inflammation in children under 16.
- “Idiopathic” means that the doctors don’t yet know the exact cause, though the inflammation comes from an autoimmune response — where the body’s immune system mistakenly attacks its own joints.
- For a diagnosis, the arthritis must have lasted at least 6 weeks.
Types of JIA
JIA isn’t one-size-fits-all — it’s an umbrella term with 7 subtypes:
- Oligoarticular JIA: 4 or fewer joints affected.
- Rheumatoid factor negative polyarticular JIA: 5 or more joints affected, blood test for rheumatoid factor (RF) negative.
- Rheumatoid factor positive polyarticular JIA: 5 or more joints affected, blood test for rheumatoid factor (RF) positive.
- Enthesitis related JIA: Arthritis plus inflammation at tendon or ligament attachment sites.
- Psoriatic JIA: Arthritis accompanied by a psoriatic skin rash.
- Systemic JIA: Whole-body inflammation, with fevers, rash, and swollen glands.
- Undifferentiated arthritis: When the arthritis doesn’t fit other categories.
Each type has a unique pattern, age of onset, and progression. Identifying the subtype guides treatment, monitoring, and long-term care.
More on the Rheumatoid Factor Blood TestIn a rheumatoid factor (RF) blood test, the patient’s blood is analyzed for the presence of rheumatoid factor, which is an antibody.
|
RISK FACTORS FOR JIA
- While the exact cause of JIA remains unknown, some children are more genetically susceptible. Having relatives with autoimmune diseases may increase risk.
- Environmental triggers like infections, stress, or exposure to certain toxins can sometimes activate the disease in these children.
SYMPTOMS TO WATCH OUT FOR
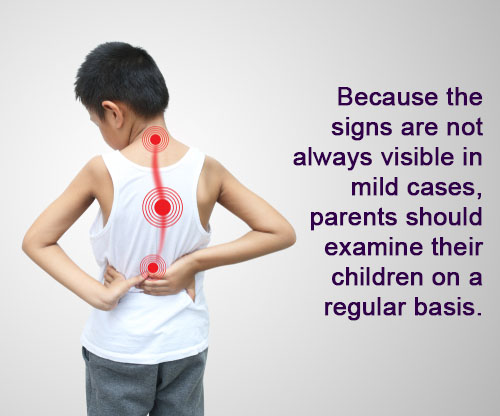
Children may adapt to discomfort, so pain isn’t always obvious.
Parents should watch for the following:
- The child avoids strenuous physical activities such as running and climbing.
- The child uses one hand more than the other.
- Limping or reduced activity.
- Swollen joints.
- Morning stiffness that eases after the child has moved around.
JIA isn’t fully curable yet, but early diagnosis and proper treatment can lead to a higher chance of remission — where the child experiences no pain, swelling, or stiffness, even when they are placed on lower doses of medications or after stopping medications.
Hence, parents should not delay bringing their child to a doctor if they suspect that their child could have developed JIA.
DIAGNOSING JIA
When parents bring their child for medical evaluation, the doctor will take a full history, examine the child thoroughly, and may order blood tests or imaging (like X-rays or ultrasounds).
Since JIA can affect the eyes, children are also referred to an eye doctor for a complete check.
TREATMENT AND MANAGEMENT OF JIA
Treatment goals include reducing inflammation in the child, offer pain relief, and protect their joints from damage.
To achieve these goals, there are several different approaches including:
- Medications. Immunosuppressive drugs can be prescribed to calm the child’s immune system.
- Physiotherapy to maintain the flexibility of the child’s joints and to prevent stiffness.
- Occupational therapy to support the child’s daily activities; splints or aids may be useful if the need arises.
- Lifestyle changes, such as daily balanced diet and gentle exercise to maintain the child’s physical strength.
Treatment Has Evolved Significantly
- Previously, non-steroidal anti-inflammation drugs (NSAIDs) and steroids were mainstays, but prolonged use risked joint damage and side effects like growth issues and weight gain.
- Disease-modifying anti-rheumatic drugs (DMARDs) allows for better disease control and reduced steroid use.
- Today, biological therapies are available to target specific immune pathways, allowing for better control of inflammation with minimal side effects. Most children can stay active, grow normally, and enjoy life.
LIVING WITH JIA
JIA can pose challenges that can affect a child’s quality of life.
- Physically, children face stiffness, pain, and fatigue, making daily tasks like dressing, writing, or climbing stairs harder.
- Hospital visits, medications, and injections can add stress.
- Steroid medications can affect appearance, impacting self-esteem.
- Emotionally, children may feel left out or anxious about the future.
Parental Support Is Key
Parents are key to helping children manage JIA.
- Educate yourself on JIA and its treatments so that you have a better understanding of what your child is going through and how to respond to your child’s problems.
- Work closely with your child’s healthcare team to maintain a consistent routine and medication plan for your child.
- Encourage gentle exercise and family participation when it comes to physical activities.
- Work with your child’s school to keep the child engaged academically.
- Provide emotional support by listening to your child and validating their feelings and concerns.
Reach Out to Support Networks
- In Malaysia, Arthritis Foundation Malaysia (AFM) (link opens in a new tab) offers a “Junior Club” with activities and educational resources.
- Internationally, Juvenile Arthritis Research (JAR) (link opens in a new tab) and Versus Arthritis (link opens in a new tab) provide guides, online resources, and communities for children and families living with JIA.
| This article is part of our series on children’s health, growth, and development. |