WORDS MAS AMIRAH MOHMAD AZHAR & DR HASLINA ABDUL HAMID
FEATURED EXPERTS
 MAS AMIRAH MOHMAD AZHAR MAS AMIRAH MOHMAD AZHAR
Student of Master’s in Clinical Nutrition
Faculty of Health Sciences
Universiti Kebangsaan Malaysia (UKM) |
 DR HASLINA ABDUL HAMID DR HASLINA ABDUL HAMID
Lecturer and Registered Dietitian Nutritionist
Centre for Community Health Studies (ReaCH)
Faculty of Health Sciences
Universiti Kebangsaan Malaysia (UKM) |
Exclusive breastfeeding is recommended for infants from birth until at least 6 months of age.
This is defined as providing an infant with just breast milk—no other foods or liquids.
For the first six months of life, the World Health Organization (WHO) and other health organizations highly advise this practice, as it can contribute to many advantages for both mother and baby.
THE BENEFITS OF BREASTFEEDING
In addition to its balanced nutritional composition, breast milk contains important substances such as immunoglobulin A or Ig A, lactoferrin, cytokines, enzymes, growth factors and leucocytes. These substances provide the baby with protection against infections while also promoting intestinal adaptation and maturation.
Breast milk also contains numerous prebiotic substances such as human milk oligosaccharides (HMO), which support the growth of non-pathogenic probiotic microorganisms, primarily lactobacilli and bifidobacteria, while removing the potentially pathogenic bacteria. This high concentration of HMO is unique to humans, and studies have shown that breastfed infant has a more stable and constant population of oligosaccharides compared with infants fed with formula milk.
Furthermore, the composition of breast milk is unique, as the concentration of both energy and protein in expressed breast milk is highly variable throughout lactation stages, between mothers, and even from the same mother.
Breast milk feeding also has been linked to improved long-term neurocognitive development and cardiovascular health outcomes.
Additionally, numerous studies have demonstrated the effectiveness of breast milk in offering protection even to preterm infants in the Neonatal Intensive Care Unit (NICU).
THE JUGGLE BETWEEN BABY AND BRIEFCASE
For many working mothers, balancing work and breastfeeding can be challenging.
If you’re one of these mothers, you can choose to breastfeed exclusively or partially once you go back to work.
If you choose to exclusively breastfeed, you should express your milk while you’re on your work breaks. You can use this expressed milk to build up a supply for the feeding of your infant by a caregiver while you’re at work or for moments when you face a shortage of breast milk.
TIPS & ADVICE
The following may be useful for working mothers that still wish to breastfeed as well as to support needs of their infants.
Don’t stress yourself out!
While it’s always ideal to aim to complete your breastfeeding journey until 2 years, you and your health matters too.
Studies have shown that the benefits of breast milk on babies are dose-dependent, so the more and the longer you give, the better the beneficial effects are.
With that said, it also means that some breast milk is better than none.
Every drop matter, so while you are trying your best to pump your milk within your capacity, do not be discouraged by the amount. You might get to express more in some days and just a little in other days, and it’s totally fine.
Seek help whenever necessary.
Being a new mother is overwhelming with both love and new responsibilities, so it is very important for you to prioritise your mental and physical well-being.
Also, go for consistent health check-ups and give yourself ample time to rest.
Know your employment policies.
Nowadays, many companies provide reasonable breaks for breastfeeding employees to express breast milk. Certain companies even provide special rooms or areas for pumping the breastmilk, which comes with a refrigerator to store breast milk as well as a wash area. These venues are kept out of sight and away from public or coworker intrusion.
You can request for such an area at your workplace if such a space is not available.
The location to express your breast milk, the number of breaks available for you, and the length of each break likely differ from company to company. You should get a better understanding on your employer’s company’s policy when it comes to expressing breast milk at the workplace. This way, you can incorporate breast milk expression into your work schedule without negatively affecting your work performance or your ability to get enough rest.
You have the right to ask for permission, explain about your timetable routines to express milk, and enquire about any accommodations to improve your ability express milk more conveniently, so don’t hesitate to talk to your supervisor or human resource department.
You can do this early, such as before your delivery date, so that you can transition from your maternity leave to back to work more seamlessly.
Manage your expectations.
Know how much you need to pump, how many sessions you need to spare your time for, and how much breast milk your baby needs.
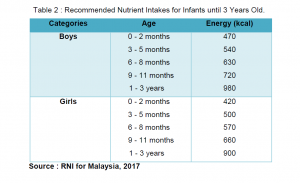
How much does your baby need? While it is quite difficult to estimate how much a baby receives from direct breastfeeding, Recommended Nutrient Intake for Malaysia 2017 states that:
- Babies need around 500 to 600 kcal/day during their first year of life.
- This amount increases to around 900 to 980 kcal/day at the age of 1 to 3 years.
The number of breastfeeding sessions is reduced as the baby ages, but the amount of milk needed by the baby is increased, from 6 to 8 sessions and 60 to 150 ml.
So, the number of pumping sessions and amount of milk needed to be expressed could be tailored to that.
The amount of milk consumed by your baby is usually reduced once you start them on complementary feeding, but they can still be breastfed on demand, with direct breastfeeding done at home.
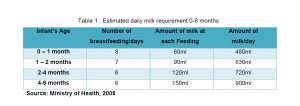
Estimated daily milk requirements of babies from 0 to 6 months old. Click image for a larger, clearer version.
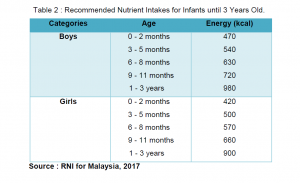
The recommended nutrient intake for infants from 0 to 3 years old. Click on the image for a larger, clearer version.
Invest in a good breast pump and breast milk storage.
There are many innovations and developments in the design of breast pumps and related accessories.
Hence, before purchasing a breast pump, take time to research by reading reviews or talking to your healthcare about the necessary equipment to meet your breastfeeding needs. You can also opt for trial or rental period to determine whether a breast pump is suitable for you.
Don’t just choose based on design and brand—you must also choose based on your needs also your budget. Local brands are usually more economical while still having comparable good quality to imported brands.
If you have a busy schedule, there are certain brands that offer quiet, wearable, or hands-free option which could accommodate your routine.
You will also need specialised storage bags made specifically to hold breast milk for safe transportation and storage.
- Look for BPA-free bags that are strong enough to be kept in the freezer or refrigerator.
- Consider bags with double zipper seal, the ability to stand alone for simple pouring, and a write-on section to record the time and date you expressed the milk.
Also, after each use of the breast pump, you should clean every area that came into contact with your breast milk or breast tissue. It is not always possible to use soap and water, particularly at work when you might not have access to a sink or have limited time. Cleansing wipes prevail for these instances!
Breastfeeding sanitizer spray is another useful consideration for quick or last-minute cleaning.
To make breast pump cleaning easier when you are on the go, make sure the supplies you buy fit compactly inside your pump bag.
Maintain proper hydration.
Have a bottle of water ready every time you pump your breast milk as well as every time you breastfeed your baby.
Water is essential, but it’s especially critical for working breastfeeding moms to stay focused and energised throughout the day.
Studies have shown that consuming more fluids than normal does not result in an increase in milk production. However, drinking too little water can lead to dehydration, which can harm your health and the quality of your breast milk.
Therefore, to ensure that your body is functioning at its best, it is crucial to consume enough fluids as to stay hydrated, which can range from 1.5 to 2.5 litres per day.
Some mothers rely on coffee to stay awake— which makes sense when your baby decided to play at 3 am! —so consuming low to moderate amounts (around 2 to 3 cups per day, or less than 300 mg of caffeine) is still considered acceptable.
Balanced meals are always key!
Recommended Nutrient Intake for Malaysia 2017 recommends that lactating mothers should consume about 2,400 kcal/day in the first 6 months of lactation, which is approximately 500 kcal more than normal adult women (1,800 to 1,900 kcal for a moderately active individual).
For mothers that want to lose some of their pregnancy weight, make sure to have adequate calories and protein according to your needs. Schedule an appointment with a dietitian if you need help to plan your meal.
Make sure to include plenty of fruits and vegetables in your meals as they are a great supply of important vitamins and minerals. Carbohydrates, especially from whole grains, is a great source of energy and fibre that can support the ability to feel full for longer.
Healthy snacking is encouraged in between meals. Go for fruit smoothies, toast, crackers, yogurt, and nuts.
TO SUM THINGS UP
Exclusive breastfeeding is one of the essential components of early childhood nutrition, but every breastfeeding mother’s circumstances are different. Therefore, it’s critical to identify a schedule and strategy that are most effective for you and your baby.
Furthermore, practice self-compassion while you manage this delicate balancing act, and don’t be afraid to seek for help and advice from your loved ones, coworkers, family members, and friends.
 FEATURED EXPERT
FEATURED EXPERT


 MAS AMIRAH MOHMAD AZHAR
MAS AMIRAH MOHMAD AZHAR DR HASLINA ABDUL HAMID
DR HASLINA ABDUL HAMID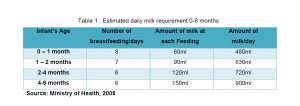

 DR NIK MUKHRIZ NIK MUSTAPHA
DR NIK MUKHRIZ NIK MUSTAPHA DR MOHD AMIR MUKHSIN ZURIN ADNAN
DR MOHD AMIR MUKHSIN ZURIN ADNAN




 DR AISHAH MOHD HAFIZ
DR AISHAH MOHD HAFIZ DR DURGA VETTIVEL
DR DURGA VETTIVEL
 AINUL SYAFIQAH MOHD AZAHARI
AINUL SYAFIQAH MOHD AZAHARI DR NUR HANA HAMZAID
DR NUR HANA HAMZAID





 FEATURED EXPERT
FEATURED EXPERT