WORDS HAMSTENI SUPPARMANIAM AND ASSOCIATE PROFESSOR DR NIK SHANITA SAFII
 FEATURED EXPERT FEATURED EXPERTHAMSTENI SUPPARMANIAM BSc Dietetics Student of Master’s in Clinical Nutrition Faculty of Health Sciences Universiti Kebangsaan Malaysia (UKM) |
 FEATURED EXPERT FEATURED EXPERTASSOCIATE PROFESSOR DR NIK SHANITA SAFII Senior Lecturer Centre for Community Health Studies (ReACH) Faculty of Health Sciences Universiti Kebangsaan Malaysia (UKM) |
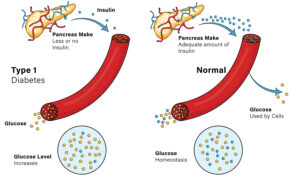
Type 1 diabetes is an autoimmune condition where the body produces little to no insulin due to the destruction of pancreatic beta cells.
It can develop at any age but is most common in children, adolescents, and young adults.
In Malaysia, misdiagnosis is common, especially in children under 5, often leading to delayed treatment.
POSSIBLE COMMON SYMPTOMS OF TYPE 1 DIABETES THAT YOU SHOULD WATCH OUT FORThese symptoms may occur over a few weeks and months.
|
WHY GOOD TYPE 1 DIABETES MANAGEMENT IS IMPORTANT
Ignoring blood sugar levels is like ignoring a car’s warning light. Eventually, something will break down!
Short-Term Risks
Diabetic ketoacidosis (DKA)
- A complication that results from increased levels of a chemical called ketones in the blood.
- It causes excessive thirst, frequent urination, fatigue, and vomiting.
- Symptoms include fruity-smelling breath, nausea, and muscle stiffness.
- This is a medical emergency and requires immediate medical attention.
Long-Term Risks
- Kidney failure (nephropathy)
- Nerve damage (neuropathy)
- Vision loss (retinopathy)
- Foot infections
To manage type 1 diabetes well and to reduce the risk of complications, a personalized plan involving doctors, dietitians, and pharmacists is key. This plan includes medications, balanced nutrition, and exercise to ensure a healthy lifestyle.
THE ROLES OF PROTEIN AND FATS IN BLOOD SUGAR MANAGEMENT
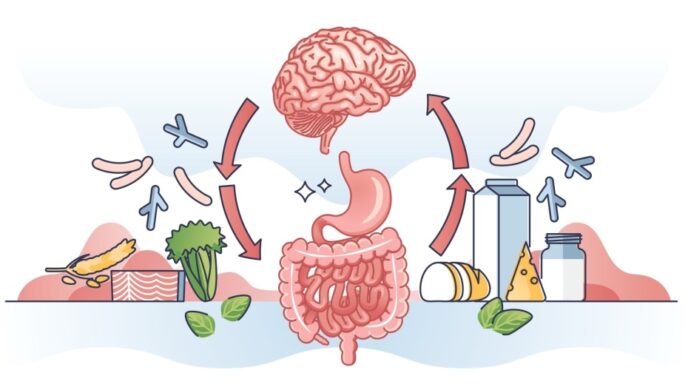
How Protein Affects Blood Sugar
- Do you know protein can raise blood sugar levels—but slowly?
- This is due to the action of glucagon, which is a hormone that helps the liver produce glucose from amino acids.
- High protein intake or fasting can cause a delayed glucose rise, typically 3 to 5 hours after eating.
- On the other hand, protein also aids in weight loss by promoting a feeling of fullness, reducing overeating.
How Fats Influence Blood Sugar
- Fat doesn’t directly convert into glucose but slows digestion, delaying blood sugar spikes.
- However, excessive fat intake, especially saturated and trans fats, can increase insulin resistance.
WITH THIS INFORMATION IN MIND, HERE’S HOW WE CAN PLAN BALANCED MEALS FOR BETTER CONTROL OF TYPE 1 DIABETES
Combining carbohydrates, fibre, protein, and fats in meals can result in:
- Smaller glucose spikes
- Longer-lasting satiety
For meals high in protein and fats, insulin adjustments may be needed to maintain stable blood sugar levels.
What Are the Ideal Amounts of Protein and Fats?
There is no universally ideal amount of protein and fat recommended for optimizing glycaemic control, so dietary goals should be personalized based on individual caloric needs.
Generally:
- Adults: Protein (15–20% of total daily calories), fats (20–35%), carbs (45–60%)
- Children and teens: Protein (15–20%), fats (30–35%), carbs (45–55%)
You should consult a dietitian to calculate how many calories you should eat and are currently eating daily, and from that point, you can also figure out the amount and types of proteins, fats, and carbs you should eat in each meal.
A Guide to Healthy Food Options
Protein options:
- Plant-based options include beans, lentils, tofu; comes with added benefits of fibre and healthy fats.
- Poultry and eggs.
- Fish, especially omega-3-rich options like salmon, and shellfish.
- Limit consumption of red meats.
Fat options:
- Choose monounsaturated fats such as olive oil, canola oil, nuts such as pumpkin seeds.
- Choose polyunsaturated fats such as sunflower oil, corn oil.
- Avoid or limit saturated fats (butter, cheese, etc) and trans fats (fast foods, deep-fried foods, processed foods).
KEY TAKEAWAYS
- Meals with a healthy balance of carbs, proteins, and fats help maintain steady blood sugar and prevent overeating.
- Protein can cause a slow glucose rise; opt for lean sources.
- Fats delay glucose absorption; prioritize unsaturated fats.
Are you ready to take control of your blood sugar with smarter food choices? A small change today could make a big difference tomorrow!
References:
- University of Hawai‘i at Mānoa Food Science and Human Nutrition Program and Human Nutrition Program (2020, August 26). Digestion and absorption of lipids. In Human nutrition: 2020 edition. Pressbooks. https://pressbooks.oer.hawaii.edu/humannutrition2/chapter/5-digestion-and-absorption-of-lipids/
- University of Hawai‘i at Mānoa Food Science and Human Nutrition Program and Human Nutrition Program (2020, August 26). Protein digestion and absorption. In Human nutrition: 2020 edition. Pressbooks. https://pressbooks.oer.hawaii.edu/humannutrition2/chapter/6-protein-digestion-and-absorption/
- American Diabetes Association (2011). Diagnosis and classification of diabetes mellitus. Diabetes care, 34 Suppl 1(Suppl 1), S62–S69. https://doi.org/10.2337/dc11-S062
- American Diabetes Association. (n.d.). Best protein choices for diabetes. https://diabetes.org/food-nutrition/reading-food-labels/protein
- American Diabetes Association. (2023, October 2). The importance of protein for people with diabetes. https://diabetesfoodhub.org/blog/importance-protein-people-diabetes
- US Centers for Disease Control and Prevention, C. (2024, May 15). About diabetic ketoacidosis. https://www.cdc.gov/diabetes/about/diabetic-ketoacidosis.html
- US Centers for Disease Control and Prevention, C. (2024, May 15). Symptoms of diabetes. https://www.cdc.gov/diabetes/signs-symptoms/index.html
- Colberg S. R. (2022). Why glucagon matters for hypoglycemia and physical activity in individuals with type 1 diabetes. Frontiers in clinical diabetes and healthcare, 3, 889248. https://doi.org/10.3389/fcdhc.2022.889248
- Freckmann, G., Hagenlocher, S., Baumstark, A., Jendrike, N., Gillen, R. C., Rössner, K., & Haug, C. (2007). Continuous glucose profiles in healthy subjects under everyday life conditions and after different meals. Journal of diabetes science and technology, 1(5), 695-703. https://doi.org/10.1177/193229680700100513
- García-López, J. M., González-Rodriguez, M., Pazos-Couselo, M., Gude, F., Prieto-Tenreiro, A., & Casanueva, F. (2013). Should the amounts of fat and protein be taken into consideration to calculate the lunch prandial insulin bolus? Results from a randomized crossover trial. Diabetes technology & Therapeutics, 15(2), 166-171. https://doi.org/10.1089/dia.2012.0149
- Holt, R. I. G., DeVries, J. H., Hess-Fischl, A., Hirsch, I. B., Kirkman, M. S., Klupa, T., Ludwig, B., Nørgaard, K., Pettus, J., Renard, E., Skyler, J. S., Snoek, F. J., Weinstock, R. S., & Peters, A. L. (2021). The management of type 1 diabetes in adults. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia, 64(12), 2609–2652. https://doi.org/10.1007/s00125-021-05568-3
- Iizuka, K., & Yabe, D. (2023). Dietary and nutritional guidelines for people with diabetes. Nutrients, 15(20), 4314. https://doi.org/10.3390/nu15204314
- Institute of Medicine. (2005). Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein, and amino acids. The National Academies Press. https://doi.org/10.17226/10490
- Ogle, G.D., Fei, W., Gregory, G.A., & Maniam, J. (2022). Type 1 diabetes estimates in children and adults. International Diabetes Federation. https://diabetesatlas.org/idfawp/resource-files/2022/12/IDF-T1D-Index-Report.pdf
- Kahanovitz, L., Sluss, P. M., & Russell, S. J. (2017). Type 1 diabetes – a clinical perspective. Point of care, 16(1), 37–40. https://doi.org/10.1097/POC.0000000000000125
- Langin D. (2011). In and out: Adipose tissue lipid turnover in obesity and dyslipidemia. Cell metabolism, 14(5), 569–570. https://doi.org/10.1016/j.cmet.2011.10.003
- Lucier, J., & Mathias, P. M. (2024). Type 1 diabetes. In StatPearls. StatPearls Publishing.
- Mavinkurve, M., Jalaludin, M. Y., Chan, E. W. L., Noordin, M., Samingan, N., Leong, A., & Zaini, A. A. (2021). Is misdiagnosis of type 1 diabetes mellitus in Malaysian children a common phenomenon?. Frontiers in endocrinology, 12, 606018. https://doi.org/10.3389/fendo.2021.606018
- Pancheva, R., Zhelyazkova, D., Ahmed, F., Gillon-Keren, M., Usheva, N., Bocheva, Y., Boyadzhieva, M., Valchev, G., Yotov, Y., & Iotova, V. (2021). Dietary intake and adherence to the recommendations for healthy eating in patients with type 1 diabetes: A narrative review. Frontiers in nutrition, 8, 782670. https://doi.org/10.3389/fnut.2021.782670
- Paterson, M., Bell, K. J., O’Connell, S. M., Smart, C. E., Shafat, A., & King, B. (2015). The role of dietary protein and fat in glycaemic control in type 1 diabetes: Implications for intensive diabetes management. Current diabetes reports, 15(9), 61. https://doi.org/10.1007/s11892-015-0630-5
- Paterson, M. A., Smart, C. E. M., Lopez, P. E., McElduff, P., Attia, J., Morbey, C., & King, B. R. (2016). Influence of dietary protein on postprandial blood glucose levels in individuals with type 1 diabetes mellitus using intensive insulin therapy. Diabetic medicine, 33(5), 592-598. https://doi.org/https://doi.org/10.1111/dme.13011
- Shwide-Slavin, C. (2003). Case study: A patient with type 1 diabetes who transitions to insulin pump therapy by working with an advanced practice dietitian. Diabetes spectrum, 16(1), 37-40. https://doi.org/10.2337/diaspect.16.1.37
- Smart, C. E., Annan, F., Higgins, L. A., Jelleryd, E., Lopez, M., & Acerini, C. L. (2018). ISPAD Clinical Practice Consensus Guidelines 2018: Nutritional management in children and adolescents with diabetes. Pediatric diabetes, 19 Suppl 27, 136–154. https://doi.org/10.1111/pedi.12738
- World Health Organization. (2023). WHO guidelines approved by the Guidelines Review Committee. In Saturated fatty acid and trans-fatty acid intake for adults and children: WHO Guideline [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK594769/