Menopause can bring more than hot flashes and mood swings. Many women experience changes in their vaginal and urinary health due to lower oestrogen levels. Dr Premitha Damodaran explains vulvovaginal atrophy, a common but under-recognized part of genitourinary syndrome of menopause, its symptoms, and the practical steps women can take to feel comfortable again.
WORDS LIM TECK CHOON
 FEATURED EXPERT FEATURED EXPERTDR PREMITHA DAMODARAN Consultant Obstetrician and Gynaecologist Pantai Hospital Kuala Lumpur |
GENITOURINARY SYNDROME (GSM) OF MENOPAUSE
“Genitourinary syndrome of menopause, or GSM, is a term introduced in 2014 to cover the range of changes menopause causes in the vulva, vagina, and urinary tract,” Dr Premitha Damodaran tells us.
- Previously, conditions like vulvovaginal atrophy (VVA) — mainly vaginal dryness — were considered separate from other conditions linked to menopause.
- GSM also includes issues such as urinary frequency, urgency, incontinence, and recurrent urinary infections.
- By placing these issues under GSM, a healthcare provider can offer a more holistic and comprehensive care to a woman having these issues.
The article focuses on vulvovaginal atrophy, the most common GSM complaint.
VULVOVAGINAL ATROPHY (VVA) IN CLOSER DETAIL
Sometimes referred to as just vaginal atrophy, VVA which refers to the thinning, drying, and inflammation of the vaginal walls due to reduced oestrogen.
“Because of menopause, the skin in the vaginal and vulvar area becomes very thin, similar to how the skin on our hands and legs thins over time,” Dr Premitha explains.
How Vulvovaginal Atrophy Happens
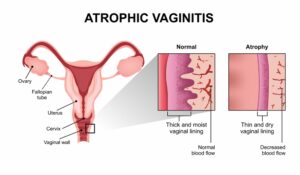
- Oestrogen plays a key role in maintaining the vaginal lining, moisture, and the balance of the bacterial population, mainly Lactobacillus, on the lining.
- When oestrogen levels drop due to menopause, pre-menopause, or even postpartum while breastfeeding, the vaginal skin thins, moisture decreases, and the protective bacteria decline.
The bacterial population of the vaginal lining, also called the vaginal flora, plays a few important roles:
Dr Premitha explains that this why women are encouraged to just use plain water and mild unscented soap to clean the external “lips” of their vagina, the vulva. This practice avoids disrupting the vaginal flora. |
YOU MAY HAVE VVA IF YOU EXPERIENCE THESE SYMPTOMS
- Vaginal dryness and burning
- Itchiness, even without infection
- Pain or discomfort in the vaginal area during exercise or daily activities
- Pain or discomfort during sexual activity; the entrance or vulva may even bleed
- Painful urination; urine can sometimes irritate the thinned vaginal lining
- Recurrent vaginal or urinary infections
Dr Premitha notes that VVA can affect even women who are not sexually active, as they can experience significant burning and itching that affects their quality of life.
“The discomfort can persist day and night, demoralizing the woman,” she adds.
DON’T SUFFER IN SILENCE, SEE A DOCTOR
Aside from keeping the pain and itch under check, Dr Premitha points out that there are other possible, more serious, issues that can cause symptoms similar to VVA.
- One example is lichen sclerosus, which can affect women during menopause but requires a different type of treatment.
- If post-menopausal bleeding is also present, the doctor needs to run some investigations to rule out cancer.
Dr Premitha says, “We cannot assume dryness is due to menopause. Examination is key. Sometimes, the solution is very simple — moisturizing the area — but proper evaluation is essential.”
TREATMENT OPTIONS FOR VVA
Lifestyle Adjustments and Self-Care First
Simple steps taken at home can help to keep the pain and itch under control, such as:
- Avoid hot water and harsh soaps when cleaning the vulva; use room-temperature water and, if necessary, mild unscented soap.
- Wear loose underwear to aerate the area when possible; you can even ditch the underwear and go commando at home.
- Moisturize the vulvar area regularly with non-perfumed moisturizers, similar to hand care.
- Adjust exercise routines to minimize friction or chafing in the vaginal area. Cycling, for example, can be switched out for a more low-impact swimming; make sure to dry and moisturize the vulvar area after.
- Reduce sugar intake, which may also help overall skin health.
Topical Therapies
- Vaginal moisturisers with hyaluronic acid can be used twice a week to restore moisture down there.
Hormone Therapies
- Vaginal oestrogen (available as pills, gels, or sprays) specifically targets the vaginal tissue and can be helpful.
- There is no need for additional progestogen therapy.
According to Dr Premitha, initially one may have to initially apply the hormones every day, but over time, the frequency will be reduced to once or twice a week.
- She emphasizes that VVA is a condition that will persist for the rest of one’s life, so hormone therapies are also long-term in nature.
- Treatment initially focuses on rebuilding vaginal tissues, hence the more frequent at first.
- Eventually, treatment will focus on maintenance to keep the vaginal lining healthy. During this phase, hormone therapy is still necessary.
Can Probiotics Help?
|
IN CONCLUSION
Vulvovaginal atrophy and GSM are common, but women often do not seek medical attention because of embarrassment or the assumption that their discomfort is a “natural” part of ageing.
This is unfortunate, because early intervention can prevent further complications as well as allow a woman to still lead a full, active, and enjoyable life after menopause.
Thus, Dr Premitha tells us: “Don’t hesitate to see a doctor. Many women are shy to discuss these issues, but with guidance, simple lifestyle changes, moisturizers, or targeted hormone therapies can make a big difference.”
| This article is part of our series on how to lead a healthy and fulfilling life during menopause. |









