WORDS LIM TECK CHOON
 FEATURED EXPERT FEATURED EXPERTPROFESSOR DR NAZIMAH IDRIS Medical Director IMU Healthcare |
I’m still young. Should I be concerned about menopause at this point in time?
“We should speak to women long before they reach menopause, so that, when it happens, they are more prepared and less anxious about it,” says Professor Dr Nazimah Idris.
She adds: “Many women I see wish they had known earlier what they could have done to prepare themselves. As every woman will go through this experience, you should enter this life phase empowered with knowledge.”
What’s menopause, exactly?
According to Prof Dr Nazimah, menopause is when a woman’s ovaries stop producing eggs and she stops menstruating.
Medically, menopause is confirmed when a woman has not experienced menstruation after one year.
Generally, this takes place when a woman is between 45 and 55 years old.
About 5% of women worldwide, however, experience early menopause between the ages of 40 and 45.
It’s also possible to experience menopause after undergoing a hysterectomy, chemotherapy, and other medical procedures that can damage the ovaries and affect menstruation.
Why do some women experience symptoms of menopause even when they are still menstruating?
Prof Dr Nazimah explains that this is likely because the woman is experiencing perimenopausal stage (often called perimenopause for short), which can occur even before a woman enters menopause.
This stage usually lasts 4 to 5 years.
“During this time, it is normal to have irregular menstruation that may include heavier bleeding as well as infrequent or skipped cycles,” she elaborates.
Perimenopause can occur due to changes in a woman’s endocrine system. These changes can cause a reduction in the levels of oestrogen, the female sex hormone.
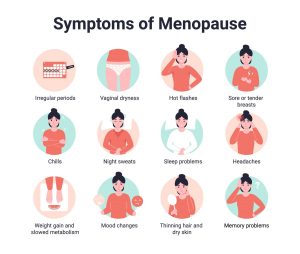
Because of this reduction in levels, a woman may experience symptoms of menopause such as hot flashes, fluctuating emotional states, difficulty sleeping and vaginal dryness.
She may also experience forgetfulness, low energy levels and reduced libido which, combined with vaginal dryness, can lead to less interest in sex and intimacy.
Once the woman enters menopause, the symptoms can become more severe and last up to another 5 years.
That sounds uncomfortable. Can anything be done about it?
Prof Dr Nazimah admits that a woman going through perimenopause and later menopause may experience around 10 years of symptoms. “This is a long time to be coping with symptoms if they are disrupting your daily life.”
Hormone therapy can help to manage severe and disruptive symptoms.
Tell me more about hormone therapy. Does it work, and how does it work?
“Hormone therapy can be very helpful in relieving hot flashes and improving sleep quality, vaginal dryness and urinary incontinence, among others,” she says.
There are different types of hormone therapy: tablets, topical creams, vaginal ring, and more. Medications may also be prescribed when necessary, such as to reduce the risk of osteoporosis due to low levels of oestrogen in the body.
The doctor will recommend the most suitable option based on a woman’s needs, family history, and other factors.
This sounds intriguing. Is hormone therapy an option for every woman experiencing symptoms of menopause?
Well, for one thing, Prof Dr Nazimah points out that hormone therapy is generally well-tolerated.
Hence, it is an option available to most women even when they have chronic diseases such as type 2 diabetes and high blood pressure.
However, hormone therapy may not be suitable for women that have certain diseases and conditions such as breast cancer, liver disease, thromboembolism, and heart disease.
If you have a health condition and are interested in hormone therapy, Prof Dr Nazimah recommends consulting a doctor for more information.
 FEATURED EXPERT FEATURED EXPERTSIN YEN SUAN Certified Chinese Medicine Practitioner IMU Healthcare |
How about natural remedies for menopause symptoms? Do they work?
According to Sin Yen Suan, a certified Chinese medical practitioner, natural remedies such as evening primrose and black cohosh are traditionally turned to for perimenopause and menopause.
However, research on the efficacy on these remedies has yet to uncover any conclusive evidence on their efficacy in relieving the symptoms of perimenopause and menopause.
“However, Chinese medicine may be able to help,” Yen Suan offers.
She explains that the effectiveness of Chinese medicine can be seen by about 3 cycles of treatment, although the whole treatment process for menopause symptoms may last 1 to 2 years.
How exactly can Chinese medicine help?
Yen Suan further elaborates that Chinese medicine treat health problems by addressing imbalances in the body through individualized therapies, based on each person’s health status, needs, and other factoers.
“Many women come to me for help with symptoms such as persistent or heavy vaginal bleeding especially, heavy sweating, hot flashes, and disturbed sleep,” she says. “To help, we use several different treatments such as herbal medications to balance their qi or acupuncture to stimulate blood flow at the meridian points. These methods help to ease their emotional state, so they are able to feel better and sleep better at night.”
Chinese medicine can complement a person’s current Western medicine regime. If you are considering Chinese medicine to complement your current medical treatments, she recommends keeping both your doctor and Chinese medicine practitioner updated on your current forms of treatment.
| PROF DR NAZIMAH’S TO-DO CHECKLIST FOR WOMEN EXPERIENCING MENOPAUSE |
|



 FEATURED EXPERT
FEATURED EXPERT