One in ten women of reproductive age suffer from this painful condition, yet many remain undiagnosed for years. Dr Inbajoothi Veeramuthu explains everything you need to know about endometriosis — from early warning signs to modern treatment options that can transform your quality of life.
WORDS DR INBAJOOTHI VEERAMUTHU
 FEATURED EXPERT FEATURED EXPERTDR INBAJOOTHI VEERAMUTHU Consultant Obstetrician and Gynaecologist Columbia Asia – Batu Kawan |
WHAT EXACTLY IS ENDOMETRIOSIS?
Endometriosis is a chronic or long-term inflammatory condition that affects the female reproductive system.
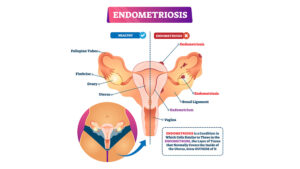
To understand it simply:
- Imagine the tissue that normally lines the inside of your uterus (called the endometrium) somehow grows in places where it should not be, such as on your ovaries, fallopian tubes, or other areas in your pelvis.
- This misplaced tissue behaves just like the lining in your uterus, thickening and bleeding with each menstrual cycle.
- However, unlike menstrual blood that can exit the body, this blood has nowhere to go.
- As a result, it will cause inflammation, pain, and sometimes scarring.
HOW DO YOU KNOW IF YOU HAVE ENDOMETRIOSIS?
The symptoms of endometriosis can vary greatly from woman to woman.
Surprisingly, about 20 to 25% of women with the condition experience no symptoms at all!
However, the most common warning signs include:
- Severe menstrual pain (dysmenorrhea) that worsens over time and may not respond well to regular painkillers.
- Chronic pelvic pain that intensifies before your period begins.
- Pain during intercourse (dyspareunia), particularly with deep penetration.
- Difficulty in getting pregnant despite trying for an extended period.
- Some women also experience digestive issues, fatigue, and pain during bowel movements or urination, especially during menstruation.
WHO TENDS TO DEVELOP ENDOMETRIOSIS?
Endometriosis most commonly affects women between the ages of 18 and 45, essentially throughout the childbearing years.
It is not limited to teenagers, and many women receive their diagnosis well into their twenties, thirties, or even forties.
RISK FACTORS THAT INCREASES YOUR RISK OF DEVELOPING ENDOMETRIOSIS
Certain factors can make you more likely to develop endometriosis:
- Family history of the condition
- Being taller than average
- Having shorter menstrual cycles
- Starting your periods at an early age
- Regular alcohol consumption
- High caffeine intake
PROTECTIVE FACTORS AGAINST ENDOMETRIOSIS
Interestingly, some lifestyle factors appear to lower the risk:
- Regular exercise
- Using oral contraceptives
- Having a higher body mass index
- Consuming omega-3 fatty acids regularly
- Smoking (though this is not recommended due to other health risks)
HOW TO MANAGE THE PAIN
When dealing with endometriosis pain, especially if you are not trying to conceive, several effective first-line treatments are available:
- Non-steroidal anti-inflammatory drugs (NSAIDs) can help manage pain and inflammation
- Combined hormonal contraceptives (birth control pills containing both oestrogen and progestin) help to regulate hormones
- Progestin-only options such as dienogest, medroxyprogesterone acetate injections, or the levonorgestrel intrauterine device (a hormone-releasing IUD)
If these first-line treatments are not sufficient, your doctor may consider second-line therapies including:
- Gonadotropin-releasing hormone (GnRH) agonists, which are medications that temporarily suppress ovarian function
- GnRH antagonists
- Aromatase inhibitors
WHEN SURGERY IS NECESSARY
Surgery is not always the first option for endometriosis.
The decision requires careful consideration of your symptoms, life goals, and fertility plans.
The Surgical Approach
Surgery works best when combined with ongoing medical management. There are two main types:
Conservative surgery
- Preserves fertility.
- Involves removing or destroying endometrial implants, addressing deep infiltrating endometriosis, and removing endometriomas (ovarian cysts caused by endometriosis).
Definitive surgery
- Includes hysterectomy (removal of the uterus) or oophorectomy (removal of ovaries).
- This should only be considered as a last resort when other treatments have failed and you do not wish to preserve fertility.
Important Considerations
- Women considering surgery should understand that multiple surgeries carry long-term risks.
- It is crucial to discuss all available treatment options, including pain management and hormonal therapies, with the doctor before opting for repeated surgical procedures.
Can One Develop Endometriosis Again After Surgery?
Unfortunately, endometriosis can return after surgery.
This is why medical treatment plays a crucial role in preventing recurrence and controlling symptoms long-term.
Endometriosis typically requires ongoing medical suppression, as symptoms and the disease itself may return if treatment is discontinued.
- Oral contraceptives and progesterone therapy have proven effective in reducing symptom recurrence.
- However, they cannot help women who are actively trying to conceive.
- Therefore, individual responses to treatment can vary significantly.
FERTILITY OPTIONS FOR WOMEN WITH ENDOMETRIOSIS
For women with endometriosis who are struggling to conceive, several options can improve the chances of pregnancy.
Surgical Benefits for Fertility
- Research shows that removing endometrial implants can improve fertility outcomes compared to managing symptoms alone.
- Laparoscopic surgery — minimally invasive surgery using small incisions — generally produces better conception rates than traditional open surgery (laparotomy).
Success Rates by Severity
- Mild endometriosis (stages 1 and 2): Women may see an 8.6% increase in conception rates in the year following surgery compared to no intervention.
- Moderate to severe endometriosis (stages 3 and 4): Without treatment, pregnancy rates can be as low as 33% for stage 3 and 0% for stage 4. However, laparoscopic surgery can improve these rates significantly,
- Stage 3: 57-69% pregnancy rates after surgery.
- Stage 4: 52-68% pregnancy rates after surgery.
THE PATH FORWARD
Endometriosis is a complex condition that affects each woman differently.
The key to successful management lies in working closely with your healthcare provider to develop a personalized treatment plan that addresses your specific symptoms, fertility goals, and quality of life priorities.
Remember, you do not have to suffer in silence. With proper diagnosis and treatment, most women with endometriosis can effectively manage their symptoms and lead fulfilling lives.
If you suspect you might have endometriosis, do not hesitate to speak with a gynecologist who can guide you through the available options and help you find relief.
| This article is part of our series on tips and advice on matters related to a woman’s health. |