WORDS NURUL HUDA SHAMSURI AND DR NOR AINI JAMIL
 FEATURED EXPERT FEATURED EXPERTNURUL HUDA SHAMSURI Master’s Student in Clinical Nutrition Faculty of Health Sciences Universiti Kebangsaan Malaysia |
 FEATURED EXPERT FEATURED EXPERTDR NOR AINI JAMIL Senior Lecturer Centre for Community Health Studies (ReaCH) Faculty of Health Sciences Universiti Kebangsaan Malaysia |
Malaysia, with its year-round sunshine, seems an unlikely hotspot for vitamin D deficiency.
Yet, over half of Malaysians experience insufficient levels of this essential nutrient.
Despite the abundant sunlight, lifestyle habits, cultural practices and dietary limitations prevent many from benefiting fully from the ‘sunshine vitamin’.
WHY DO WE NEED VITAMIN D?
- Vitamin D is vital for maintaining strong bones by regulating calcium levels, thereby helping to prevent falls and fractures.
- It is associated with reduced risks of chronic conditions such as high blood pressure, diabetes, cancer, autoimmune diseases and infections.
HOW CAN WE OBTAIN OUR VITAMIN D?
- Vitamin D is primarily synthesized when the skin is exposed to ultraviolet-B (UVB) rays from sunlight.
- Some amounts can be obtained from foods such as fatty fish (salmon, mackerel, sardines, etc), meat, egg yolks, mushrooms and fortified products such as milk and margarines.
- However, foods naturally rich in vitamin D are limited and not commonly consumed in Malaysian diets, leaving sunlight as the main source for most people.
THE CHALLENGES IN GETTING OPTIMAL AMOUNTS OF VITAMIN D
Some Groups Are More at Risk
Certain groups are more vulnerable to vitamin D deficiency in Malaysia, including:
- Children and adolescents
- Women
- Urban residents
- Indoor workers
- Individuals with obesity
Among our ethnic groups, Indians and Malays are at higher risk due to:
- Darker skin pigmentation, which reduces vitamin D synthesis
- Cultural and religious practices, such as wearing clothing that covers most of the body
Urbanization
Urbanization can worsen the problem, with many people spending most of their time indoors or commuting in vehicles.
Malaysians’ Attitude About Sun Exposure
Additionally, many Malaysians avoid sun exposure due to a lack of knowledge about vitamin D, concerns over skin health, a preference for fair skin and busy lifestyles.
Their misconceptions significantly limit their sun exposure, thus increasing the risk of vitamin D deficiency.
GETTING ENOUGH SUNLIGHT EXPOSURE IS KEY
In Malaysia, vitamin D-rich foods are limited, supplements are rarely consumed, and food fortification with vitamin D is not mandatory.
Hence, sunlight remains the most accessible and cost-effective source of this essential vitamin.
Maximizing Vitamin D Synthesis Requires Exposing as Much Skin as Possible for a Short Time
- Minimal exposure, such as exposing just the face, prolongs the time needed and increases the risk of skin damage.
- While dietary sources and supplements can help to fulfill vitamin D requirements, completely avoiding sunlight is not ideal for maintaining good health.
- Striking a balance between sun safety and vitamin D needs is key to reaping its full benefits.
Safe sun exposure offers additional benefits beyond vitamin D production, including:
|
However, Ensuring Sufficient Sun Exposure Is Not Straightforward
Various factors influence vitamin D synthesis, including:
- UVB intensity
- Time of day
- Air pollution
- Skin type
- Age
- Outdoor exposure duration
- The amount of skin exposed
Currently, Malaysia does not have official sun exposure guidelines. In their absence, recommendations from the Australian Skin and Skin Cancer Research Centre (ASSC) offer practical strategies to safely optimize sun exposure for vitamin D synthesis while minimizing risks.
RECOMMENDATIONS FOR SAFE SUN EXPOSURE
The balance of the risks and benefits of sun exposure varies between individuals according to skin type and underlying risk of skin cancer. Skin types can be classified using Fitzpatrick scale, which indicate varying levels of susceptibility to sunburn.
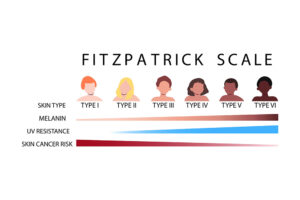
Skin Types I and II (High Risk of Skin Cancer)
- Pale skin that burns easily and tans minimally
- Sun protection:
- Apply sunscreen when the UV index is 3 or higher, and wear protective clothing, sunglasses and hats.
- Sun protection is unnecessary when the UV index is below 3, unless exposure exceeds 2 hours.
- Vitamin D tips:
- Spend a few minutes of morning sunlight on unprotected skin.
- Incorporate dietary sources of vitamin D or supplements as required.
Skin Types III and IV (Intermediate Risk of Skin Cancer)
- Light to medium brown skin that sometimes burns and can develop a moderate-to-deep tan with repeated exposure to the sun.
- Sun protection:
- Apply sunscreen when the UV index is 3 or higher.
- Brief exposure can help maintain adequate vitamin D levels as long as enough skin is exposed.
- For longer outdoor exposure, use protective measures such as long sleeves, sunglasses and hats.
- Sun protection is usually unnecessary when the UV index is below 3, unless exposure exceeds 2 hours.
- Vitamin D tips:
- Spend less than 10 minutes outdoors with 35% of the body exposed (such as by wearing a short-sleeved t-shirt and shorts).
- If only 10% of the body is exposed (such as by wearing long trousers and an elbow-length shirt), increase exposure time to about 20 minutes.
Skin Types V and VI (Low Risk of Skin Cancer)
- Deeply pigmented brown to black skin that rarely or never burns.
- Sun protection:
- Routine sunscreen use is not needed, but prolonged exposure (over 2 hours) under a UV index 3 or higher requires sunscreen and protective measures.
- Vitamin D tips:
- Spend time outdoors most days with some skin exposed.
- This group requires 2 to 4 times more sun exposure than lighter skin types to produce sufficient vitamin D.
This article is part of our series on tips and advice for leading a healthy lifestyle.
|
References:
- Mohd Saffian, S., Jamil, N. A., Mohd Tahir, N. A., & Hatah, E. (2022). Vitamin D insufficiency is high in Malaysia: A systematic review and meta-analysis of studies on vitamin D status in Malaysia. Frontiers in nutrition, 9, 1050745. https://doi.org/10.3389/fnut.2022.1050745
- Jamil, N. A., Yew, M. H., Noor Hafizah, Y., Gray, S. R., Poh, B. K., & Macdonald, H. M. (2018). Estimated vitamin D synthesis and dietary vitamin D intake among Asians in two distinct geographical locations (Kuala Lumpur, 3°N v. Aberdeen, 57°N) and climates. Public health nutrition, 21(17), 3118–3124. https://doi.org/10.1017/S1368980018002057
- Chin, K. Y., Ima-Nirwana, S., Ibrahim, S., Mohamed, I. N., & Wan Ngah, W. Z. (2014). Vitamin D status in Malaysian men and its associated factors. Nutrients, 6(12), 5419–5433. https://doi.org/10.3390/nu6125419
- Abd Aziz, N. H., Yazid, N. A., Abd Rahman, R., Abd Rashid, N., Wong, S. K., Mohamad, N. V., Lim, P. S., & Chin, K. Y. (2020). Is first trimester maternal 25-hydroxyvitamin D level related to adverse maternal and neonatal pregnancy outcomes? A prospective cohort study among Malaysian women. International journal of environmental research and public health, 17(9), 3291. https://doi.org/10.3390/ijerph17093291
- Shahudin, N. N., Sameeha, M. J., Mat Ludin, A. F., Manaf, Z. A., Chin, K. Y., & Jamil, N. A. (2020). Barriers towards sun exposure and strategies to overcome these barriers in female indoor workers with insufficient vitamin D: A qualitative approach. Nutrients, 12(10), 2994. https://doi.org/10.3390/nu12102994
- Quah, S. W., Abdul Majid, H., Al-Sadat, N., Yahya, A., Su, T. T., & Jalaludin, M. Y. (2018). Risk factors of vitamin D deficiency among 15-year-old adolescents participating in the Malaysian Health and Adolescents Longitudinal Research Team Study (MyHeARTs). PloS one, 13(7), e0200736. https://doi.org/10.1371/journal.pone.0200736
- Shafinaz, I. S., & Moy, F. M. (2016). Vitamin D level and its association with adiposity among multi-ethnic adults in Kuala Lumpur, Malaysia: A cross sectional study. BMC public health, 16, 232. https://doi.org/10.1186/s12889-016-2924-1
- Farrar, M. D., Webb, A. R., Kift, R., Durkin, M. T., Allan, D., Herbert, A., Berry, J. L., & Rhodes, L. E. (2013). Efficacy of a dose range of simulated sunlight exposures in raising vitamin D status in South Asian adults: implications for targeted guidance on sun exposure. The American journal of clinical nutrition, 97(6), 1210–1216. https://doi.org/10.3945/ajcn.112.052639
- Jamil, N. A., Shahudin, N. N., Abdul Aziz, N. S., Jia Qi, C., Wan Aminuddin, W. A. A., Mat Ludin, A. F., Chin, K. Y., Abd Manaf, Z., & Mat Daud, N. (2019). Knowledge, attitude and practice related to vitamin D and its relationship with vitamin D status among Malay female office workers. International journal of environmental research and public health, 16(23), 4735. https://doi.org/10.3390/ijerph16234735
- Neale, R. E., Beedle, V., Ebeling, P. R., Elliott, T., Francis, D., Girgis, C. M., Gordon, L., Janda, M., Jones, G., Lucas, R. M., Mason, R. S., Monnington, P. K., Morahan, J., Paxton, G., Sinclair, C., Shumack, S., Smith, J., Webb, A. R., & Whiteman, D. C. (2024). Balancing the risks and benefits of sun exposure: A revised position statement for Australian adults. Australian and New Zealand journal of public health, 48(1), 100117. https://doi.org/10.1016/j.anzjph.2023.100117
- Considering cosmetic procedures? Know your Fitzpatrick skin type first. (2023, August 30). Enrich Clinic. https://www.enrichclinic.com.au/what-is-fitzpatrick-skin-type/