Heartburn can be terrifying. Many people assume that they are having heart problem, but when the issue is something else. Though it feels similar, heartburn is actually digestive issue, not a cardiac one. A gastroenterologist explains why.
WORDS LIM TECK CHOON
 FEATURED EXPERT FEATURED EXPERTDR CHIENG JIN YU Consultant Physician, Gastroenterologist and Hepatologist Pantai Hospital Ampang |
IS THAT A BURNING IN YOUR HEART?
Heartburn is a term used to describe an uncomfortable, sometimes painful sensation in the chest, at the back of the breastbone. It feels as if your heart is on fire, hence the name.
However, the heart has nothing to do with heartburn!
Instead, it is a condition that affects the area where your oesophagus—the tube-like muscular structure that carries food down your throat to the stomach—meets the stomach.
In fact, the medical term for frequent heartburn is gastroesophageal reflux disease or GERD.
HEARTBURN HAPPENS WHEN ACID IN THE STOMACH FIND ITS WAY BACK UP TO THE OESOPHAGUS
Your stomach produces acid called gastric acid or stomach acid. This acid is needed because the enzymes in the stomach would only be able to digest foods in an acidic environment.
Now, there is a band of muscles called the sphincter that will tighten up and close the opening connecting your oesophagus and your stomach once all foods have made their way inside your stomach.
Occasionally, something goes wrong, such as the sphincter doesn’t work as it should or you develop hiatus hernia (we’ll talk more about that later). When this happens, gastric acid can flow back up to the oesophagus.
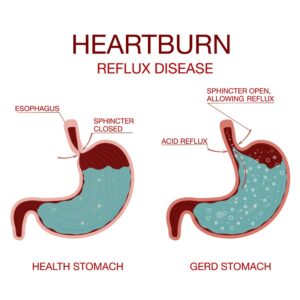
Dr Chieng Jin Yu shares that this flowing back up of the stomach acid is called a ‘reflux’, and it is responsible for heartburn sensations.
Heartburn sensation can be more intense when you’re lying down or bending over, because these positions only help keep the acid in the oesophagus for a longer period!
You May be Experiencing a Reflux if You Experience:
|
HEARTBURN IS OFTEN CONFUSED WITH GASTRITIS
“Yes, many patients will claim that they have ‘gastritis’ when they are experiencing classical GERD symptoms,” says Dr Chieng.
A study conducted by a team of investigators from University of Malaya reported in 2004 that the general prevalence of GERD in Malaysia is about 13.4%.
GERD IS LINKED TO OESOPHAGITIS OR INFLAMMATION OF THE OESOPHAGUS
Dr Chieng shares that, from the same study, it was found that about 20% of people with GERD also have severe (grades C and D) oesophagitis.
| Oesophagitis is the inflammation or irritation of the oesophagus, the tube-like organ that carries the food from the mouth down to the stomach. |
In fact, GERD is the most common cause of oesophagitis. This is because frequent exposure to stomach acids can cause the oesophageal lining to develop inflammation and ulceration.
SEE A DOCTOR WHEN HEARTBURN IS FREQUENT & INTENSE ENOUGH TO DISRUPT YOUR EVERYDAY ACTIVITIES
An occasional heartburn is usually nothing to be concerned about, but frequent heartburn or heartburn that affect your daily activities should warrant a visit to the doctor.
According to Dr Chieng, the doctor will refer you to a gastroenterologist, especially if you also experience problems swallowing or pain while swallowing.
Certain groups of people have a higher risk of developing complications from GERD. If you fall under any of these groups, you will also be referred to a gastroenterologist for further investigation.
People That Are More Prone to Developing GERD Complications
|
IF LEFT UNTREATED, GERD MAY GIVE RISE TO MORE SERIOUS HEALTH COMPLICATIONS
Dr Chieng shares that these complications include:
- Oesophagitis as described earlier
- Barrett’s oesohagus
- Oesophageal cancer
HOW GERD IS MANAGED
Medications
Dr Chieng says that one such group of medications is called proton pump inhibitors or PPI.
- These medications work on structures in the stomach called proton pumps.
- Proton pumps produce gastric acid, so these medications can stop the action of most of the proton pumps in the stomach.
- As a result, while gastric acid is still produced, it is now in smaller amounts—just enough for digestion, without aggravating GERD symptoms.
Not everyone responds to PPI, however, so other types of medications, such as the latest called potassium-competitive acid blockers or PCAB can be considered.
Antidepressants may be prescribed if you experience emotional issues due to the disruptions in your life as a result of your GERD.
Surgery
Some people develop GERD due to hiatus hernia.
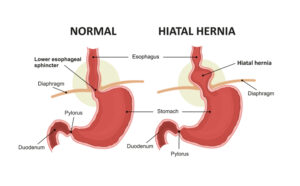
Hiatus hernia, also called hiatal hernia, occurs when there is a hole in the diaphragm, and your stomach protrudes through this hole into the middle compartment of your chest.
Surgery can be performed to treat this hernia. Dr Chieng says that these days, such surgery can be guided using an endoscope, a flexible tube with a light source and camera at one end.
“Unfortunately, GERD symptoms may recur in about 50% of patients that have undergone such surgery,” Dr Chieng adds.
Lifestyle Modifications
While the full list of lifestyle changes may change from one person to another, due to factors such as age, gender, health status, etc, the most common recommendations are:
- Raise the head of the bed to reduce GERD symptoms while sleeping. A study, published in 2012, recommends raising the head of the bed by 20 cm.3
- If you’re overweight, lose the excess weight.
- Avoid excessive alcohol.
- Stop smoking.
- Avoid having heavy evening meals or nighttime snacks.
- Avoid consumption of foods high in fat.
- Avoid foods that can irritate your oesophagus and stomach such as coffee, chocolate, citrus, carbonated drinks, peppermint, and spicy foods. Consult your doctor for a more thorough list of dos and don’ts when it comes to these foods.

This article is part of our series on foods and how consuming these foods can affect various aspects of our health.
|
References:
- Rosaida, M. S., & Goh, K. L. (2004). Gastro-oesophageal reflux disease, reflux oesophagitis and non-erosive reflux disease in a multiracial Asian population: a prospective, endoscopy based study. European journal of gastroenterology & hepatology, 16(5), 495–501. https://doi.org/10.1097/00042737-200405000-00010
- Fass, R., & Sifrim, D. (2009). Management of heartburn not responding to proton pump inhibitors. Gut, 58(2), 295–309. https://doi.org/10.1136/gut.2007.145581
- Khan, B. A., Sodhi, J. S., Zargar, S. A., Javid, G., Yattoo, G. N., Shah, A., Gulzar, G. M., & Khan, M. A. (2012). Effect of bed head elevation during sleep in symptomatic patients of nocturnal gastroesophageal reflux. Journal of gastroenterology and hepatology, 27(6), 1078–1082. https://doi.org/10.1111/j.1440-1746.2011.06968.x