Compared to haemodialysis, peritoneal dialysis offers a flexible alternative for individuals with chronic kidney disease who need a treatment option that easily fits into their busy schedules and lifestyle, even at home.
WORDS DR THEEPA NESAM M.R. AND LIM TECK CHOON
 FEATURED EXPERT FEATURED EXPERTDR THEEPA NESAM M.R. Consultant Nephrologist and Physician Sri Kota Specialist Medical Centre |
| This article is long, but this is because we provide details of everything you need to know about peritoneal dialysis—the types available, how they work, the advantages, the downsides, and more. We believe that if you read on, you’ll find this a most informative article. |
WHAT EXACTLY IS PERITONEAL DIALYSIS?
Peritoneal dialysis, often abbreviated as PD, is a type of treatment for kidney failure that uses the lining of your abdomen, called the peritoneum, as a natural filter.
The Peritoneum at a Glance
- The peritoneum is a thin, slippery membrane that lines the inside of your abdomen.
- This membrane covers most of the organs in that region, such as your stomach, liver, and intestines.
- It acts as a protective layer that helps keep everything in place and provides a smooth surface for your abdominal organs to move easily against each other as you move or digest food.
- It also plays a role in protecting these organs from infections and storing excess fat.
- The peritoneum is also permeable—certain substances can pass through it. This property makes it useful in peritoneal dialysis.
HOW DOES PD WORK?
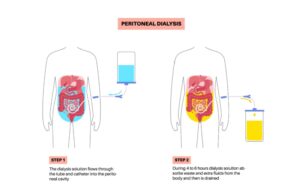
- A catheter is surgically implanted into the abdomen about 2 weeks before initiation of PD.
- The procedure of doing peritoneal dialysis is referred to as an exchange. Every exchange comprises 3 stages: fill, dwell, and drain.
- Fill
- Sterile dialysis fluid is introduced into the abdominal cavity via the catheter. The fluid contains sugar, water, and electrolytes sodium, potassium, and calcium.
- Dwell
- Excess fluid and wastes are transferred into the dialysis solution or dialysate.
- Drain
- After certain amount of time, the dialysate, now containing the waste products, is drained from your abdomen.
The entire process above is typically repeated several times a day.
| A catheter is a soft, flexible tube used to insert the dialysate into the abdomen and drain it out during peritoneal dialysis. The catheter stays in the abdomen and allows dialysis to be done at home. |
BETWEEN HAEMODIALYSIS AND PERITONEAL DIALYSIS, WHICH IS THE RIGHT CHOICE FOR ME?
| Haemodialysis is a treatment that filters waste, toxins, and excess fluids from your blood when your kidneys cannot perform this function. During the process, blood is drawn, ‘cleaned’ as it moves through the haemodialysis machine, and then returned to your body, typically through a vein. |
Both peritoneal dialysis and haemodialysis (HD) are treatments for kidney failure, but they function in different ways.
Haemodialysis

- Method. Uses a machine with a semipermeable membrane to filter the blood.
- Location. Typically requires regular trips to a dialysis centre.
- Frequency. Typically done 3 to 4 times a week, for several hours per session.
- Comfort. Can be less comfortable due to needle insertions and the long duration of each session.
- Duration. Can be time-consuming, which can limit certain activities.
- Potential complications. Risks include hypotension (low blood pressure), muscle cramps, and access site complications.
Peritoneal Dialysis
- Method. Uses the body’s own peritoneum, a membrane lining the abdomen, as a natural filter.
- Location. Can be performed at home, work, or even while traveling.
- Frequency. Multiple exchanges are usually done daily, including overnight.
- Comfort. Often considered more comfortable, as it doesn’t involve needles.
- Duration. Offers more flexibility in daily activities.
- Potential complications. Risks include peritonitis (infection of the peritoneum), hernia, and fluid overload.
Ultimately, the best choice between peritoneal dialysis and haemodialysis hinges on individual factors such as lifestyle, health status, and personal preferences.
It’s important to discuss these options with a nephrologist to determine the most suitable treatment.
PD IS OFTEN RECOMMENDED IN THE FOLLOWING SITUATIONS
To Preserve Residual Renal Function
- Residual renal function refers to the ability of the kidney of people with end-stage kidney disease to eliminate water and toxins.
- For people with end-stage kidney disease that still have residual renal function, PD helps to preserve this function better than haemodialysis.
- Preserving residual renal function is associated with better fluid balance, reduced morbidity, and improved survival.
For Flexibility, Convenience, and a Greater Sense of Control and Normalcy
- PD is a home-based therapy, suitable for patients with limited or no access to haemodialysis centres.
- Elderly patients or those with mobility limitations may benefit, especially if they have caregivers or family members that can assist with replacing used dialysate with fresh ones.
- Fewer dietary and fluid restrictions compared to haemodialysis.
- Allows patient to maintain a sense of normalcy, privacy, and control over their treatment.
For Younger, Active Patients and Children
- PD is less disruptive compared to haemodialysis.
- Can be integrated into daily school or work and social routines with minimal disruption.
- An option for younger patients who may need long-term dialysis and want to avoid using up early their vascular sites.
| Vascular sites are locations on the body where a tube or needle is connected to blood vessels for dialysis to be performed. |
Patients With Cardiovascular Issues Such as:
Cardiovascular instability
- A condition in which a person’s cardiovascular functions become unreliable, insufficient, or otherwise problematic, often due to an underlying condition such as high blood pressure.
- Those with severe cardiac disease or unstable blood flow (haemodynamic) may tolerate PD better because it avoids the rapid fluid shifts seen in haemodialysis.
Severe high blood pressure and/or congestive heart failure
- PD provides more gradual fluid removal.
- This reduces the risk of worsening heart failure or uncontrolled hypertension.
Low blood pressure (hypotension)
- PD is less likely to cause episodes of low blood pressure due to its continuous nature.
People with Issues with Their Blood Vessels
PD does not involve insertion of needles into blood vessels.
Hence, it is:
- Suitable for people whose vein is difficult to be found and used by the doctor or nurse.
- Suitable for people with complicated blood vessel structure (unusually positioned, narrow, twisted, etc).
- Suitable for people that are unable to undergo medical procedures that involve insertions of needles and other devices into their blood vessels.
Patients That Cannot Tolerate Haemodialysis, Such as:
- People that experience bleeding and other adverse effects when given anticoagulants during haemodialysis.
- People that experience adverse reactions when undergoing haemodialysis (headaches, muscle cramps, etc).
- People that are unable to undergo medical procedures that involve insertions of needles and other devices into their blood vessels.
Those That Are Awaiting Renal Transplant
- PD is often preferred for patients on the renal transplant list.
- It may help maintain better haemodynamic stability and residual renal function.
- This can improve post-transplant outcomes.
THERE ARE 2 TYPES OF PD
#1 Continuous Ambulatory Peritoneal Dialysis (CAPD)

- You connect the dialysate fluid bag to the catheter and allow it to infuse into your abdomen.
- The fluid remains in your stomach for around 4 to 6 hours. During this period, you may move about and perform the majority of your routine activities.
- Subsequently, you evacuate the fluid from your abdomen.
- You subsequently introduce fresh dialysate into your abdomen.
- This process of draining and refilling usually takes 30 to 40 minutes. It should be performed around 4 times daily.
- The process of draining and refilling the stomach requires approximately 30 to 40 minutes.
#2 Automated Peritoneal Dialysis (APD)
- A machine fills and drains the fluid from your belly. The machine is sometimes called a ‘cycler’.
- The exchange procedure requires approximately 8 to 12 hours.
- This means that you can perform APD during the night while you sleep.
- Modern APD machines have advanced sensors and automated programming that allow precise control over the fill, dwell, and drain phases.
- These machines are also more compact, quieter, and user-friendly, thereby improving the patient’s experience, especially during overnight therapy.
- Many APD machines have with customizable programming options that allow physicians to tailor the dialysis regimen to the patient’s specific needs.
- While APD is more flexible and convenient compared to CAPD, it costs more than CAPD.
THE DOWNSIDES OF PD
Risk of Peritonitis
- Peritonitis is a common complication caused by bacterial or fungal infections of the peritoneal cavity.
- It can result from contamination during exchanges or due to a malfunctioning catheter.
- Symptoms include abdominal pain, fever, cloudy dialysate, and nausea.
- Recurrent or severe peritonitis may require switching to haemodialysis.
Catheter-Related Complications
- Infections at the catheter exit site or along the subcutaneous tunnel can occur, potentially leading to peritonitis or the need to replace the catheter.
- The catheter may become blocked, dislodged, or malfunction, causing issues with fluid drainage and requiring surgical intervention.
Protein Loss and Malnutrition
- PD can lead to the loss of proteins and amino acids into the dialysate, which may contribute to protein-energy wasting and malnutrition over time.
- This is particularly concerning in patients with poor nutritional status or those that cannot maintain adequate dietary intake.
Metabolic Complications
- The glucose-based solutions used in PD can lead to hyperglycaemia, especially in diabetic patients. This can result in poor glycaemic control and contribute to long-term complications.
- Absorption of glucose from the dialysate can contribute to weight gain and dyslipidaemia, necessitating close monitoring and possible dietary or medication adjustments.
Fluid Overload and Dehydration
Mismanagement of the dialysis prescription can lead to either:
- Fluid overload, causing hypertension, oedema, or heart failure.
- Dehydration, resulting in hypotension, dizziness, or electrolyte imbalances.
Mechanical Complications
- Increased intra-abdominal pressure from the presence of dialysate fluid can cause or worsen abdominal or inguinal hernias, especially in older patients or those with weak abdominal walls.
- Leakage of dialysate through the catheter site or into the pleural cavity (pleuroperitoneal leak) can occur, leading to suboptimal dialysis and the need for temporary cessation of PD.
Encapsulating Peritoneal Sclerosis (EPS)
- A rare but serious complication of long-term PD, it is characterized by progressive thickening and fibrosis of the peritoneal membrane.
- EPS can lead to bowel obstruction, malnutrition, and cessation of PD.
Peritoneal Membrane Changing over Time
- Prolonged exposure to hypertonic solutions and glucose degradation products can lead to structural and functional changes in the peritoneal membrane.
- These changes can reduce the effectiveness of the membrane and potentially leading to ultrafiltration failure.
Patient and Caregiver Burden
- PD requires active patient involvement and meticulous attention to sterile technique during exchanges.
- This can be challenging for elderly patients, those with physical or cognitive impairments, or those lacking social support.
- Patients or caregivers need training and must be willing to perform exchanges consistently, which can be demanding and may affect their quality of life.
FORTUNATELY, ADVANCES IN PD TECHNOLOGY HAVE GONE A LONG WAY IN ADDRESSING THESE ISSUES
Useful Advances in APD Technology
- APD machines with advanced sensors and automated programming for precise control of fill.
- Customizable APD software to tailor the dialysis regimen to the patient’s specific needs and treatment goals.
- Newer PD cyclers with connectivity features to transmit treatment data to healthcare providers in real time, for remote monitoring and early detection of complications.
- Many PD systems support telemedicine platforms, enabling healthcare providers to conduct virtual consultations and provide timely interventions.
Useful Dialysate Innovations
| Just to recap: dialysate is the special fluid used in dialysis to help remove waste, toxins, and extra water from the blood. In peritoneal dialysis, it is put into the abdomen to absorb these unwanted substances before being drained out. |
- Icodextrin and amino acid-based dialysates for patients who require long-dwell exchanges or those with diabetes. These solutions help reduce the glucose load, prevent weight gain, and improve fluid management.
- Biocompatible dialysates, with lower concentrations of glucose degradation products and neutral pH, to minimize peritoneal membrane damage and reduce the incidences of peritonitis and peritoneal membrane fibrosis.
- New dialysates with better electrolyte balance to help address issues like acidosis, improve patient comfort, and enhance ultrafiltration.
- Improvements in the packaging of dialysate solutions and the availability of pre-packaged sterile PD systems to reduce contamination risks during exchanges.
| This article is part of our series on tips and advice for keeping the kidneys healthy. |