WORDS LIM TECK CHOON
 FEATURED EXPERT FEATURED EXPERTDR KHOO CHING SOONG Consultant Internal Medicine Physician & Neurologist Columbia Asia Hospital – Puchong |
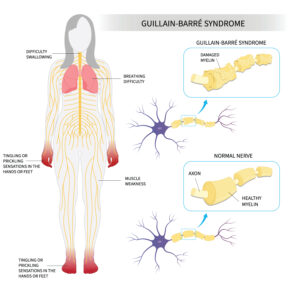
Imagine waking up one morning with a strange tingling in your toes.
By nightfall, you struggle to stand.
Within days, your body may become completely paralyzed.
This is the terrifying reality of Guillain-Barré Syndrome or GBS, a rare but serious condition that can strike suddenly and without warning.
WHAT IS GUILLAIN-BARRÉ SYNDROME (GBS)?
Dr Khoo Ching Soong, a consultant neurologist, reveals that:
- GBS is a disorder that affects the immune system.
- Instead of protecting the body, the immune system attacks the nerves that control movement and detection of sensations such as pain, temperature, and touch.
POTENTIAL SIGNS OF GBS THAT YOU SHOULD NOT IGNOREMost GBS patients only realize something is wrong when they experience sudden paralysis. However, Dr Khoo reveals that early warning signs can appear before things escalate, such as:
“If you notice these symptoms, seek medical help immediately,” advises Dr. Khoo. “Early intervention is crucial.” |
WHO IS AT RISK OF GBS?
GBS doesn’t discriminate, as it can affect people of all ages.
- While cases in Malaysia are not widely documented, Dr. Khoo notes that GBS is more common in adults and in males, with an incidence rate of 1 to 2 cases per 100,000 people per year worldwide.
- Contrary to some personal accounts, there is no evidence that GBS is becoming more prevalent among younger Malaysians.
- In fact, the incidence of GBS increases with age, particularly after 50.
THE POTENTIAL TRIGGERS OF GBS
Dr Khoo points out that, to date, we haven’t been able to pinpoint the specific cause(s) of GBS.
Common possible triggers include:
- Respiratory infections
- Stomach flu
- Viral infections
- Campylobacter jejuni, a bacteria that typically causes diarrhea
- In rare cases, even certain vaccines have been linked to GBS, though the risk is extremely low
HOW DO DOCTORS DIAGNOSE GBS?
GBS can sometimes resemble other neurological disorders such as spinal cord injury, botulism, myasthenia gravis to name a few.
Hence, making an accurate diagnosis is critical.
Doctors typically perform the following:
- Physical examination to check for muscle weakness and reflex loss.
- Nerve conduction studies (NCS) to assess nerve function.
- Lumbar puncture or spinal tap to examine cerebrospinal fluid for elevated protein levels.
IS THERE A CURE?
While there is no direct cure for GBS, Dr Khoo tells us that treatment can speed up recovery and reduce complications.
In Malaysia, two key treatments are available.
Intravenous Immunoglobulin (IVIg)
- This is a therapy that helps block harmful immune responses.
- Antibodies from donors are administered through a drip into the blood stream of the person with GBS.
- This is a proven effective treatment, although the effectiveness can vary from one individual with GBS to another.
Plasmapheresis
- Blood is first extracted from the person with GBS.
- The blood is then broken down in a special device, which separates the component of the blood that contains antibodies called the plasma from the rest of the blood.
- Next, the antibodies that attack the nerves are filtered out of the plasma.
- The ‘purified’ plasma is then administered back into the person with GBS.
- Some studies suggest that plasmapheresis works best when it is initiated early, typically within 7 days after the symptoms appear. However, this treatment can still be beneficial when initiated up to 4 weeks after the symptoms appear.
“Both treatments are available in major public and private hospitals, but access may be limited to tertiary healthcare centers,” Dr Khoo adds.
These treatments are conducted by a neurologist or a physician trained in neurology.
CAN ONE FULLY RECOVER FROM GBS AFTER TREATMENT?
The good news is that most people with GBS can recover.
“Patients typically start improving within 2 to 3 weeks after treatment,” says Dr. Khoo.
He adds: “However, recovery can take months or even years, and some patients may experience lasting weakness or fatigue.”
Factors that can affect recovery include:
- The patient is of an older age
- The symptoms are very severe, requiring admission of the patient into the intensive care unit (ICU)
- Past cases of diarrhoea
- The need for mechanical ventilation
- Weakness in the upper limbs
For those left with residual weakness, rehabilitation (including physical, occupational, and speech therapy) is crucial for them to improve their quality of life.
| A small percentage of people with GBS that have successfully undergone treatment may experience a relapse in the future. |
THE ROAD TO RECOVERY
The recovery process from GBS can be physically, mentally, and emotionally challenging.
Dr Khoo emphasizes that patients often need ongoing support, including:
- Physical therapy to rebuild their muscle strength and improve their mobility
- Pain management strategies
- Psychosocial support for both patients and their families
Fortunately, the patient and their loved ones can work closely with their healthcare team to receive such support. For example, a rehabilitation specialist can supervise the patient’s physical therapy, while counsellors or psychologists can help provide emotional support.
IN CONCLUSION
- While GBS is rare, its effects can be devastating.
- If you or someone you know experiences sudden tingling or weakness, don’t wait.
- Seek medical attention immediately, as early diagnosis and treatment can make all the difference.
| This article is part of our series on issues that affect our nerves and other components of our nervous system such as our brain and spinal cord. |