Vertigo is one of Alfred Hitchcock’s more well-known psychological thrillers, named thus because the protagonist suffered from that condition as well as fear of heights. Unfortunately, the popularity of that movie led some to assume that vertigo, dizziness and fear of heights are all one and the same!
WORDS LIM TECK CHOON
 FEATURED EXPERT FEATURED EXPERTPROFESSOR DATO’ DR BALWANT SINGH GENDEH Senior Consultant Ear, Nose, and Throat (ENT) Surgeon Pantai Hospital Kuala Lumpur |
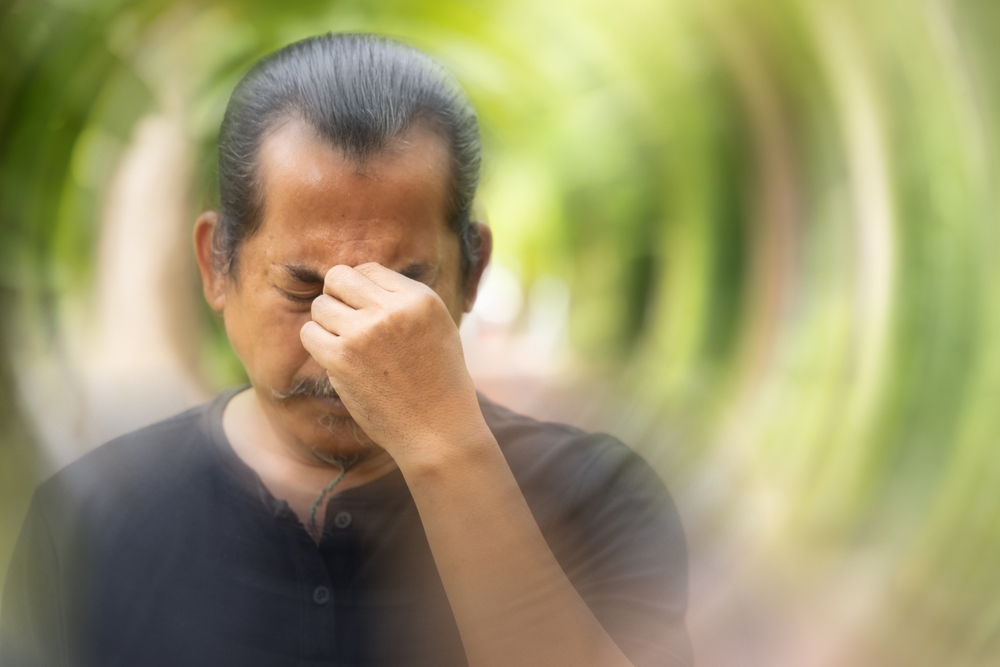
“Vertigo specifically refers to a feeling of disorientation because we think that we, or the world around us, are moving, when we are actually not,” explains Professor Dato’ Dr Balwant Singh Gendeh.
It should not be confused with motion sickness and dizziness.
IT’S LINKED TO OUR EARS, NOT OUR BRAIN
In the past, it was assumed that vertigo was a sign that something was not quite right with the brain.
Now, we know that the affected area is the inner part of the ear that helps maintain our sense of balance.
Vertigo Is a Symptom, Not an Illness
Vertigo is viewed as a symptom of a problem that affects the inner ear.
Therefore, the duration and severity of vertigo can vary, depending on the problem that gives rise to it.
To Better Understand Vertigo, Let’s Take a Closer Look at How Our Ear Affects Our Balance
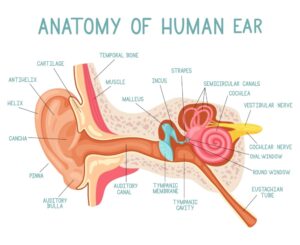
If we look at the image above, there is a structure resembling a snail with a big head located in the
inner ear.
This “snail” is called the bony labyrinth, and like its name would suggest, its outer wall is composed of rigid bony layers to protect the soft tissue inside.
There are three components of the bony labyrinth:
- Cochlea
- Three semicircular canals
- Vestibule
The semicircular canals and the vestibule work closely together with other parts of our body such as the eyes and the nerves as well as bones to help maintain our position, whether we are staying still or in motion.
Semicircular canals
- They are filled with a fluid called endolymph.
- Each canal also has a cup-like structure called cupula.
- Every time we move, the endolymph also flows in the direction of the movement, and this movement is detected by thin hairlike cells in the inner lining of the cupula.
- These cells then generate signals, sent via nerve cells, to the brain.
Vestibule
- The vestibule has thin hair-like cells, found in the utricle and saccule.
- These cells help to detect movements in a straight line as well as acceleration in a horizontal direction.
- Additionally, the utricle and succule has a jelly-like covering lined with tiny calcium crystals.
- Whenever we tilt our head or change our body’s position with respect to gravity (such as when we lie down), the calcium crystals get displaced in the direction of the movement and cause the hair-like cells to bend.
- These hair-like cells then send signals to the brain informing it about the change in our body’s
position.
Our brain pieces the information received from the inner ear together with information sent through our eyes, skeletal system, etc, in order to coordinate the maintenance of our sense of balance.
THREE COMMON ISSUES LINKED TO VERTIGO
Professor Dr Balwant will now delve into three common issues associated with vertigo, but we should keep in mind that there are several other possible conditions that may give rise to vertigo as one
of the symptoms.
These include injuries and trauma, conditions that cause a sudden decrease in blood supply to the brain such as clots in a blood vessel and more.
Therefore, if we experience bothersome or frequent bouts of vertigo, it’s a good idea to consult an ENT specialist for a more thorough examination.
#1 Benign Paroxysmal Positioning Vertigo (BPPV)
- BPPV is the most common form of vertigo.
- “During a BPPV episode, we experience a sudden, brief sensation that we are spinning,” explains Professor Dr Balwant.
- An episode is normally triggered by specific changes in our head’s position, such as when we tilt our head or when we sit upright after lying down to sleep.
- BPPV can spur mild to intense dizziness that may last for a for a short period of time (a few seconds to a
minute).
Is it serious?
- BPPV is rarely serious, and the affected person’s hearing will not be affected.
- However, Dr Balwant cautions that the elderly may be more prone to falls should they experience a BPPV episode.
- Given how falls may lead to life-threatening fractures among people in that age group, he advises those affected to consult an ENT specialist if the episodes are frequent.
What causes it?
- BPPV could be due to the calcium crystals in utricule getting dislodged and finding their way into a semicircular canal.
- Once in the semicircular canal, these crystals interfere with the flow of the endolymph and make the brain think that we are moving when we are actually staying still.
Diagnosing BPPV
- No sophisticated equipment is necessary. This is because when our head is moved into a position that triggers the BPPV, the brain will let us know that we are moving (when we actually aren’t) and our eyes react by moving in a specific pattern known as “nystagmus”.
- Thus, during the diagnosis process, the ENT specialist will ask for the patient to move their head into various positions while watching for signs of nystagmus.
How do we treat it?
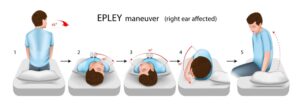
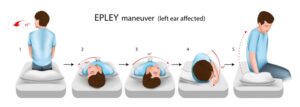
- The ENT specialist will instruct us on a series of gradual positioning techniques called the Epley maneuver.
- This technique is designed to allow the dislodged crystals in the semicircular canal to find their way back to the utricle.
- We will also be asked to come back a week later for a follow-up examination.
- If the episodes are intense, anti-vertigo medications may also be prescribed.
#2 Labyrinthitis or Vestibular Neuronitis
- Infection can occur in one of the two nerves that connect the inner ear with the brain, called the vestibular nerves.
- Such infection can give rise to a condition known as labyrinthitis or vestibula neuronitis.
Is it serious?
- Professor Dr Balwant shares that people affected by labyrinthitis typically experience vertigo alongside dizziness, nausea, and even loss of hearing.
- The hearing loss is normally temporary, but in very rare cases, it may become permanent.
- These symptoms tend to occur abruptly, without warning, often after sudden movements of the head, and they may last for several days.
- While these symptoms are normally not life-threatening, they can be intense and uncomfortable to undergo. They also disrupt our ability to work, drive and perform other routine activities.
What causes it?
- It can be due to infection of the inner ear.
- It can also be brought upon by infection of other parts of the body, such as the lungs, stomach, etc.
- We are more susceptible to such infections if we smoke, drink excessive amounts of alcohol, or indulge in other activities that can weaken our immune system.
- Allergies and stress may also be risk factors.
How do we treat it?
- The specialist will prescribe medications based on the cause of the infection.
- Bacterial infection, for example, can be treated with antibiotics, but infections caused by viruses will require a different type of treatment.
- Therefore, the specialist will evaluate the best treatment options on a case by case basis.
- In the meantime, we should take plenty of rest and drink plenty of water to help us recover faster.
#3 Ménière’s Disease
- Ménière’s disease is quite rare, with studies reporting the prevalence rate as ranging from
3.5 per 100,000 people to 513 per 100,000. - This rarity will be small consolation to those affected by this disease, however, as the symptoms tend to be severe.
Usually only one ear is affected, and the affected person can experience episodic attacks, during which the following typically occur:
- Vertigo. This often comes up without warning and can last from 20 minutes to several hours.
- Hearing loss. This usually comes and goes during the early stages, but over time, the affected person’s hearing loss may become permanent.
- Tinnitus. The affected person will hear persistent noise (ringing, buzzing, whistling, hissing, etc) in the ear even when there is no external sound present.
- A “full” sensation in the ear. There is build-up of pressure in the affected ear or on the side of the head where the affected ear is.
- Attacks of dizziness. Episodic attacks may occur in close succession over a few days.
Some people may also experience “brain fog”: they find it difficult to concentrate or recall things, and they are also prone to feeling fatigued and/or demotivated.
Consequently, their abilities to sustain meaningful relationships as well as to perform at work or school are affected.
What causes it?
Professor Dr Balwant shares that one theory is that Ménière’s disease is the result of excessive endolymph in the inner ear.
- Normally, the endolymph is contained within a semicircular canal by a membrane.
- When there is excessive endolymph, the resulting pressure causes the membrane to rupture.
- Now, the endolymph is rich in potassium ions, which is positively charged. When it leaks
into the surrounding space of the inner ear, it brings with it excess positive charges, which disrupt
the ability of the nerve cells in the inner ear to properly generate electrical signals to the brain.
Other researchers speculate that this disease is probably the result of blood vessels experiencing constrictions that reduce the amount of blood passing through them.
Some also theorize that Ménière’s disease may be due to viral infections, genetic abnormalities and other factors that prevent the body from regulating the amount of endolymph fluid in the inner ear.
How do we treat it?
Unfortunately, we have yet to find a cure.
Professor Dr Balwant explains that current treatment regime focuses on managing the symptoms.
- Medications can be prescribed for severe dizziness, vertigo, nausea, etc.
- Consumption of salt should be restricted to reduce the amount of fluid retained by the body; this fluid reduction will lead to a reduction of fluid volume and pressure in the inner ear.
- Smoking, caffeine, alcohol and chocolates should be avoided.
- Those experiencing emotional issues may find counselling and participation in support groups
helpful.
| This article is part of our series on asthma and how it affects a child’s health and quality of life. |
Reference: Alexander, T. H., & Harris, J. P. (2010). Current epidemiology of Meniere’s syndrome. Otolaryngologic clinics of North America, 43(5), 965–970. https://doi.org/10.1016/j.otc.2010.05.001