This article explains metabolic dysfunction-associated fatty liver disease (MAFLD) and how dietary management plays a key role in managing the condition, slowing its progression, and improving one’s health.
WORDS TAN HO LI & DR SHANTI KRISHNASAMY
 FEATURED EXPERT FEATURED EXPERTTAN HO LI Student of Master’s in Clinical Nutrition Faculty of Health Sciences Universiti Kebangsaan Malaysia (UKM) |
 FEATURED EXPERT FEATURED EXPERTDR SHANTHI KRISHNASAMY Senior Lecturer and Dietitian Centre for Diagnostic, Therapeutic & Investigative Studies (CODTIS) Faculty of Health Sciences Universiti Kebangsaan Malaysia (UKM) |
3 in 10 adults in Malaysia have metabolic dysfunction-associated fatty liver disease (MAFLD).
In Malaysia, those with MAFLD are 10 years younger when compared to the mean age of patients worldwide.
MORE ABOUT MAFLD
Metabolic dysfunction-associated fatty liver disease (MAFLD) is previously known as non-alcoholic fatty liver disease (NAFLD).
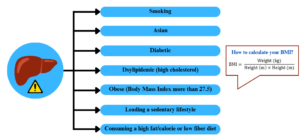
It is defined as the presence of fat buildup in the liver together along with at least one of the following:
- Overweight or obesity
- Type 2 diabetes mellitus (T2DM)
- At least 2 metabolic risk abnormalities such as:
- Waist circumference of more than 90 cm for men and 80 cm for women
- Pre-hypertension
- High cholesterol
- Low high density lipoprotein (HDL) or good cholesterol
- Pre-diabetes
HOW CAN YOU TELL IF YOU HAVE MAFLD?
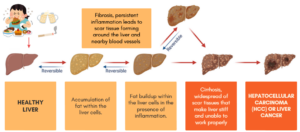
People with fatty liver usually do not show symptoms until the condition has progressed to irreversible stage of cirrhosis (see image above). This is why it is known as a silent killer!
However, some people do experience signs and symptoms, such as the following:
- Unexplained weight loss
- Pain in the upper right abdomen
- Severe fatigue and weakness
- Appetite loss
- Swollen abdomen
- Yellowing of skin and eyes
CAN MAFLD BE REVERSED?
Yes, you can if your condition is in the early stages.
The Malaysian Society of Gastroenterology and Hepatology recommend the Mediterranean diet and calorie restriction to reduce liver fat accumulation, inflammation, and stiffness.
Calorie Restriction to Induce Weight Loss
- For overweight and obese individuals, a deduction of 500-1,000 kcal from one’s daily calorie intake is recommended to induce healthy weight loss of 0.5 to 1 kg per week.
- 5 to 10% weight loss has been proven to reduce liver fat buildup and inflammation.
- Other health benefits of weight loss include:
- Improved insulin sensitivity
- Improved lipid profile
- Lower blood sugar levels
- Slowing down MAFLD progression.
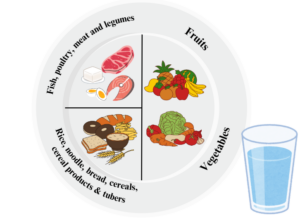
The Quarter-Quarter-Half principle of the Healthy Plate plate is an easy-to-follow guideline to ensure that you enjoy balanced main meals and control the portion sizes of these meals.
- Half the plate is allocated for fruits and vegetables. Pick fruits with lower fructose and higher fibre content such as guava, papaya and kiwi.
- One-quarter of the plate for rice, noodles, bread, cereal products, and tubers (for example, sweet potato), preferably wholegrains.
- Another one-quarter of the plate for fish, poultry, meat, egg, or legumes (for example, soybean, chickpeas, dhal, tempeh).
- Drink at least 6 to 8 glasses of plain water daily.
Mediterranean Diet
The Mediterranean diet has been shown to reduce the risk of MAFLD and slow down its progression due to its anti-inflammatory properties.
It is based on the traditional foods of countries bordering the Mediterranean Sea, such as France, Spain, Greece, and Italy.
Due to cultural differences and food preferences, some foods may not be appropriate for Malaysians. For example, the Mediterranean diet suggests consuming red wine in small servings, with a meal, and not every day, which is not applicable and appropriate to all Malaysian population, especially Muslims.
Nonetheless, the main principles of the Mediterranean diet can still be adapted to the Malaysian diet.
- Wholegrains. Choose brown rice, oats, multigrain bread and wholemeal biscuits.
- Fish that are high in omega-3 fatty acids. Indian mackerel (ikan kembong), sardines, Hoven’s carp (ikan jelawat), Barramundi (siakap), Catfish (keli), Shark catfishes (patin), Fourfinger threadfin (senangin), white pomfret.
- Healthy fats. Cashews, almonds, sunflower and pumpkin seeds
Be Physically Active
Physical activity has been proven to improve the body’s ability to break down and burn fat more efficiently, reduces fat buildup and inflammation in liver.
According to World Health Organization Physical Activity Guidelines 2020, adults are recommended to do any of the following
- At least 150 to 300 minutes of moderate-intensity aerobic physical activity
- At least 75 to 150 minutes of vigorous-intensity aerobic physical activity
- A combination of both per week
Avoid Sedentary Behaviour
The amount of time spent being sedentary such as sitting quietly in front of the TV or computer screen should be limited and replaced with physical activity of any intensity including low intensity.
Quit Smoking
- Smoking is associated with worsened liver disease progression and an increased risk for liver cancer.
- MAFLD individuals are encouraged to quit smoking by enrolling in a smoking cessation program.
Avoid Excessive Alcohol Consumption
- Alcohol consumption exacerbates liver disease progression and contributes to the accumulation of excessive fat in the abdominal area as alcohol is high in calories.
- Alcohol also worsens liver inflammation and damage.
- MAFLD individuals are encouraged to reduce or permanently stop consuming alcoholic beverages.
Go for Regular Medical Checkups and Self-Monitoring
- Discuss with your doctor about whether you need to go for liver function tests or imaging tests such as ultrasounds.
- MAFLD individuals should also monitor their blood pressure, blood sugar level, and lipid profile from time to time.
- Keep body weight records and a food diary to track your progress such as body weight changes and dietary habits.
References:
- Beygi, M., Ahi, S., Zolghadri, S., & Stanek, A. (2024). Management of metabolic-associated fatty liver disease/metabolic dysfunction-associated steatotic liver disease: From medication therapy to nutritional interventions. Nutrients, 16(14), 2220. https://doi.org/10.3390/nu16142220
- Chua, D., Low, Z. S., Cheam, G. X., Ng, A. S., & Tan, N. S. (2022). Utility of human relevant preclinical animal models in navigating NAFLD to MAFLD paradigm. International journal of molecular sciences, 23(23), 14762. https://doi.org/10.3390/ijms232314762
- Eskridge, W., Cryer, D. R., Schattenberg, J. M., Gastaldelli, A., Malhi, H., Allen, A. M., Noureddin, M., & Sanyal, A. J. (2023). Metabolic dysfunction-associated steatotic liver disease and metabolic dysfunction-associated steatohepatitis: The patient and physician perspective. Journal of clinical medicine, 12(19), 6216. https://doi.org/10.3390/jcm12196216
- Eslam, M., Newsome, P. N., Sarin, S. K., Anstee, Q. M., Targher, G., Romero-Gomez, M., Zelber-Sagi, S., Wai-Sun Wong, V., Dufour, J. F., Schattenberg, J. M., Kawaguchi, T., Arrese, M., Valenti, L., Shiha, G., Tiribelli, C., Yki-Järvinen, H., Fan, J. G., Grønbæk, H., Yilmaz, Y., Cortez-Pinto, H., … George, J. (2020). A new definition for metabolic dysfunction-associated fatty liver disease: An international expert consensus statement. Journal of hepatology, 73(1), 202–209. https://doi.org/10.1016/j.jhep.2020.03.039
- Khaznadar, F., Khaznadar, O., Petrovic, A., Hefer, M., Gjoni, F., Gjoni, S., Steiner, J., Smolic, M., & Bojanic, K. (2024). MAFLD pandemic: Updates in pharmacotherapeutic approach development. Current issues in molecular biology, 46(7), 6300–6314. https://doi.org/10.3390/cimb46070376
- European Association for the Study of the Liver (EASL), European Association for the Study of Diabetes (EASD), & European Association for the Study of Obesity (EASO) (2024). EASL-EASD-EASO clinical practice guidelines on the management of metabolic dysfunction-associated steatotic liver disease (MASLD). Obesity facts, 17(4), 374–444. https://doi.org/10.1159/000539371
- Tsigalou, C., Konstantinidis, T., Paraschaki, A., Stavropoulou, E., Voidarou, C., & Bezirtzoglou, E. (2020). Mediterranean diet as a tool to combat inflammation and chronic diseases. An overview. Biomedicines, 8(7), 201. https://doi.org/10.3390/biomedicines8070201