WORDS LIYANA TAN ABDULLAH, DR HARVINDER KAUR GILCHARAN SINGH & DR KANIMOLLI ARASU
FEATURED EXPERTS
 LIYANA TAN ABDULLAH LIYANA TAN ABDULLAH
BSc Applied Chemistry UM
Student of Master Clinical Nutrition
Universiti Kebangsaan Malaysia |
 DR HARVINDER KAUR GILCHARAN SINGH DR HARVINDER KAUR GILCHARAN SINGH
Senior Lecturer
Centre for Community Health Studies (ReaCH) Faculty of Health Sciences
Universiti Kebangsaan Malaysia (UKM) |
 DR KANIMOLLI ARASU DR KANIMOLLI ARASU
Dietitian and Senior Lecturer
IMU Division of Nutrition & Dietetics
International Medical University (IMU) |
Type 2 diabetes mellitus (T2DM) poses a significant public health challenge in Malaysia, mirroring a global trend of increasing prevalence.
According to the International Diabetes Federation (IDF), there are almost 463 million people suffering from T2DM worldwide. In Malaysia, this chronic condition is on the rise, with approximately 1 in 5 adults living with diabetes according to 2019 National Health and Morbidity Survey.
THE COST OF TREATING T2DM IN MALAYSIA IS INCREASING DAY BY DAY
Globally, total annual cost for treating diabetes in 2022 was estimated to be USD412.9 billion, which include USD306.6 billion for direct medical costs and $106.3 billion for indirect costs attributable to diabetes.
T2DM has a huge socioeconomic implication with an estimated cost of RM 4.38 billion in 2017 to treat T2DM and its complications, according to a report published by the Malaysian Ministry of Health (MOH) and the World Health Organization (WHO).
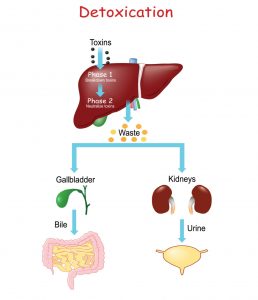
Additionally, people with T2DM suffer from complications such as heart disease, chronic kidney disease, nerve damage, vision and/or hearing problems, and mental health issues when the disease is poorly managed. Consequently, it leads to poor quality of life among Malaysians living with T2DM.
There is a need for public awareness and caution when managing T2DM. This article aims to provide comprehensive insights of the risk factors associated with T2DM and lifestyle strategies for effective diabetes management.
WHAT IS TYPE 2 DIABETES?
T2DM is a chronic health condition characterized by increased sugar (glucose) levels in the blood.
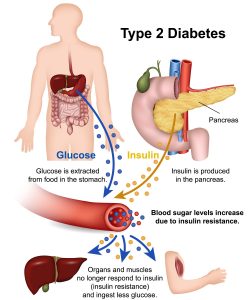
An overview of T2DM. Click on the image for a larger and clearer version.
Following a meal, our body processes the ingested food, generating sugar, specifically glucose molecules. Glucose molecules are then released into the blood stream.
Concurrently, the pancreas secretes insulin hormone to control and maintain our blood glucose level. Insulin helps our cells to utilize sugars as a source of energy for the body.
In people with T2DM, their body cannot produce sufficient insulin or there is a problem in the effective utilization of insulin. Thus, blood glucose level remains high, causing multiple complications.
RISK FACTORS OF T2DM
Various risk factors, including overweight and obesity, have been identified in association with T2DM.
Overweight and obesity
The mechanisms that link obesity with insulin resistance are still uncertain. However, some studies suggest that people with obesity have fewer insulin receptors, especially in the skeletal muscle, liver and adipose tissue, than lean people.
Excessive weight gain is posited as a potential factor contributing to the impairment of insulin function, possibly linked to the detrimental effects of fat accumulation in tissues such as the muscles and liver.
Other risk factors
Besides obesity, other risk factors for T2DM includes combination of environmental and genetic risk factors. Even though strong correlation between genetic risk factors and T2DM are found in many studies, environmental risk factors remain as crucial in the development of T2DM.
Therefore, specific strategies such as promotion of physical activity, healthy lifestyle and healthy dietary patterns combined with interventions to reduce the rate of obesity could reduce increasing number of T2DM incidences in near future.
MEALTIME STRATEGIES FOR PEOPLE WITH T2DM
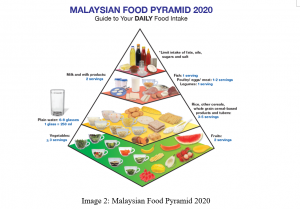
Here are some important strategies recommended by Ministry of Health Malaysia.
Portion control is crucial.
People with T2DM are recommended to have:
- 2 servings of carbohydrates for breakfast.
- 2 to 3 servings for lunch and dinner, respectively.
- 1 to 2 servings of snack.
You can use your hand as a visual guide to determine portion sizes of your foods.
| NUTRIENTS |
EXAMPLES |
SIZE OF 1 PORTION |
| Carbohydrates |
Rice |
The size of your fist. |
| Protein |
Tenggiri fish |
The size of your palm. |
| Fats |
Butter |
The size of the tip of your thumb. |
| Dietary fibre |
Green vegetables |
2 hands full. |
Additionally, you can also adhere to their specific recommended portions by following the Malaysian healthy plate such as the quarter, quarter half concept.

- Pick a dinner plate of 9-inch or 23-cm diameter.
- Fill half the plate with non-starchy vegetables, such as salad, green beans, broccoli, cauliflower, cabbage, or carrot.
- Fill one quarter with a lean protein, such as chicken, fish, turkey, beans, tempeh, tofu, or eggs.
- Fill the remaining quarter with carbohydrate-rich foods such as rice, pasta, noodles, corn, or other wholegrains. Note that a cup of milk counts as carbohydrate.
- Choose water or a low-calorie drink such as unsweetened fruit juice or tea to go with your meal.
- You can also add 2 serving of fruits per day as part of your diet.
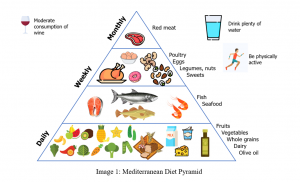
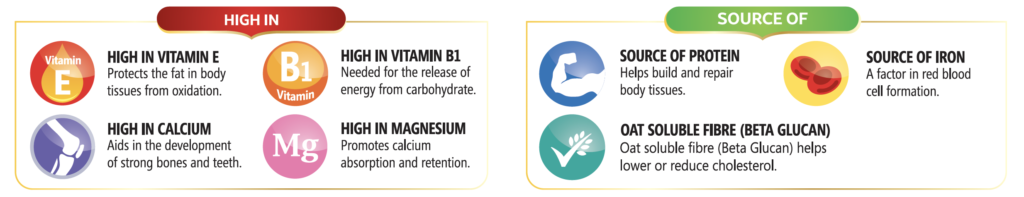
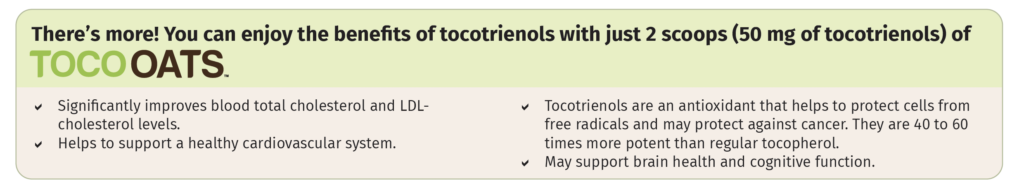
Consume high-fibre food such as fresh fruits and vegetables.
Foods containing high amounts of soluble fibres such as apples, citrus fruits, barley, and beans help to prevent sugar spikes as they slow down the digestion process.
However, these foods also contain carbohydrates and thus, you need to watch the portion sizes.
Choose wholegrains instead of simple carbohydrates.
| EXAMPLES OF SIMPLE CARBS |
EXAMPLES OF COMPLEX CARBS |
- White bread
- White pasta
- White rice
- Cakes
- Cookies
- Candy
- Ice cream
- Non-diet sodas
- Sugar cereals
- Sweetened drinks
|
- Whole wheat bread
- Brown rice
- Starchy vegetables
- Fruit
- Beans
- Lentils
- Quinoa
- Oats
- Sweet potatoes
- Chia seeds
|
Avoid or limit intake of foods high in sodium as these foods may lead to high blood pressure.
Examples of high sodium foods include salty snacks, fast food, pickles, and gravies.
Low sodium foods include whole foods such as fresh fruits and vegetables, unsalted foods or snacks, herbs and spices.
Consume healthy fats such as foods rich in unsaturated fatty acids.
Examples of fgood sources of unsaturated fatty acids include fish, nuts and seeds.
Avoid or limit intake foods high in saturated fats such as processed meat, cheese, and fatty meat.
Avoid or limit sugar sweetened beverages such as canned drinks or carbonated drinks.
These beverages add to your total calorie intake and lead to increased blood glucose levels.
People with T2DM can opt for unsweetened coffee or tea.
Avoid or limit alcohol drinks and cigarettes smoking.
Lead an active lifestyle by doing exercises.
Perform moderate-intensity exercises such as cycling less than 20km/hour, water aerobics, mowing the lawn, actively playing with children for 150 minutes per week.
Perform for at least 90 minutes per week vigorous exercise such as race walking, hiking uphill, aerobics, swimming, and cycling uphill.
Additionally, aim for at least 2 sessions per week of muscle strengthening exercises such as push-ups, squats and abdominal crunches.
Consult a healthcare professional on the appropriate types and frequency of exercise. as some individuals may need personalized exercise regime—especially the older adults, elderly and those with chronic conditions.
It is also recommended to check blood glucose levels before engaging in vigorous exercise regimes.
Consume adequate fluids to maintain good hydration status during exercise.
OTHER USEFUL TIPS
Monitoring carbohydrates intake is essential.
A dietitian can provide guidance on estimating carbohydrates intake through techniques such as carbohydrates counting or maintaining a food diary. These approaches enable people with T2DM to understand how different foods impact their blood sugar levels. It is important to pair carbohydrates counting with the blood glucose levels and medication intake.
Always monitor at home the blood sugar level for those who are at risk of hypo- or hyperglycaemia, using a blood glucose meter.
Self-monitoring of blood glucose level is important to ensure blood glucose stays within the recommended levels and it helps to prevent hypo- or hypoglycemia.
It can be done in a fasting state before and/or 2 hours after a meal.
People with T2DM should adhere to anti-diabetic medications dosage intake and insulin injection regimen to help improve blood glucose control.
Always seek guidance from healthcare professionals to manage your diabetes effectively.
Keeping a close watch on overall carbohydrates and sugar consumption remains a fundamental strategy for achieving optimal blood sugar control in people with T2DM.
Besides, people with T2DM should possess awareness and understanding of all the recommendations and guidelines provided by their healthcare professionals.
References:
- CPG Secretariat, Health Technology Assessment Section. (2020). Clinical practice guidelines: Management of type 2 diabetes mellitus (6th ed.). Ministry of Health Malaysia. https://www2.moh.gov.my/moh/resources/Penerbitan/CPG/Endocrine/CPG_T2DM_6th_Edition_2020_13042021.pdf
- Nasir, B.M., Abd. Aziz A., Abdullah, M.R., & Mohd Noor, N. (2012). Waist height ratio compared to body mass index and waist circumference in relation to glycemic control in Malay type 2 diabetes mellitus patients, Hospital Universiti Sains Malaysia. International journal of collaborative research on internal medicine & public health (IJCRIMPH), 4, 406. https://www.researchgate.net/publication/281629114_Waist_height_ratio_compared_to_body_mass_index_and_waist_circumference_in_relation_to_glycemic_control_in_Malay_type_2_diabetes_mellitus_patients_Hospital_Universiti_Sains_Malaysia
- Bener, A., Zirie, M., & Al-Rikabi, A. (2005). Genetics, obesity, and environmental risk factors associated with type 2 diabetes. Croatian medical journal, 46(2), 302–307.
- Ganasegeran, K., Hor, C. P., Jamil, M. F. A., Loh, H. C., Noor, J. M., Hamid, N. A., Suppiah, P. D., Abdul Manaf, M. R., Ch’ng, A. S. H., & Looi, I. (2020). A systematic review of the economic burden of type 2 diabetes in Malaysia. International journal of environmental research and public health, 17(16), 5723. https://doi.org/10.3390/ijerph17165723
- Gardner, C. D., Trepanowski, J. F., Del Gobbo, L. C., Hauser, M. E., Rigdon, J., Ioannidis, J. P. A., Desai, M., & King, A. C. (2018). Effect of low-fat vs low-carbohydrate diet on 12-month weight loss in overweight adults and the association with genotype pattern or insulin secretion: The DIETFITS randomized clinical trial. JAMA, 319(7), 667–679. https://doi.org/10.1001/jama.2018.0245
- Kojta, I., Chacińska, M., & Błachnio-Zabielska, A. (2020). Obesity, bioactive lipids, and adipose tissue inflammation in insulin resistance. Nutrients, 12(5), 1305. https://doi.org/10.3390/nu12051305
- Feisul, I. M., Azmi, S., Mohd Rizal, A. M., Zanariah, H., Nik Mahir, N. J., Fatanah, I., Aizuddin, A. N., & Goh, A. (2017). What are the direct medical costs of managing type 2 diabetes mellitus in Malaysia?. The medical journal of Malaysia, 72(5), 271–277.
- Shafie, A., & Ng, C.H. (2020). Estimating the costs of managing complications of type 2 diabetes mellitus in Malaysia. Malaysian journal of pharmaceutical sciences, 18, 15-32. 10.21315/mjps2020.18.2.2
- Goossens G. H. (2008). The role of adipose tissue dysfunction in the pathogenesis of obesity-related insulin resistance. Physiology & behavior, 94(2), 206–218. https://doi.org/10.1016/j.physbeh.2007.10.010
- Parker, E. D., Lin, J., Mahoney, T., Ume, N., Yang, G., Gabbay, R. A., ElSayed, N. A., & Bannuru, R. R. (2024). Economic costs of diabetes in the U.S. in 2022. Diabetes care, 47(1), 26–43. https://doi.org/10.2337/dci23-0085
 FEATURED EXPERT
FEATURED EXPERT

 TI MEI JUN
TI MEI JUN DR NURUL HUDA RAZALLI
DR NURUL HUDA RAZALLI




 ANAS ALMASWARY
ANAS ALMASWARY PROFESSOR DR SUZANA SHAHAR
PROFESSOR DR SUZANA SHAHAR
 LIYANA TAN ABDULLAH
LIYANA TAN ABDULLAH DR HARVINDER KAUR GILCHARAN SINGH
DR HARVINDER KAUR GILCHARAN SINGH DR KANIMOLLI ARASU
DR KANIMOLLI ARASU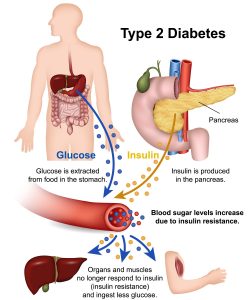


 MARAM T.M. BESAISO
MARAM T.M. BESAISO DR SHANTHI KRISHNASAMY
DR SHANTHI KRISHNASAMY

 OH YAN TING
OH YAN TING DR MUNIRAH ISMAIL (PhD)
DR MUNIRAH ISMAIL (PhD) PROFESSOR DATO’ DR ROSLEE RAJIKAN
PROFESSOR DATO’ DR ROSLEE RAJIKAN