WORDS WEDSTER SCHUMACHER ANAK KANANG, FAZRYN SHAHEERA NIZAN SHAH & DR SHANTHI KRISHNASAMY
 FEATURED EXPERT FEATURED EXPERTWEDSTER SCHUMACHER ANAK KANANG Undergraduate Student of Dietetics Programme Faculty of Health Sciences Universiti Kebangsaan Malaysia (UKM) |
 FEATURED EXPERT FEATURED EXPERTFAZRYN SHAHEERA NIZAN SHAH Undergraduate Student of Dietetics Programme Faculty of Health Sciences Universiti Kebangsaan Malaysia (UKM) |
 FEATURED EXPERT FEATURED EXPERTDR SHANTHI KRISHNASAMY Senior Lecturer and Coordinator of the Master of Clinical Nutrition Dietetics Programme Universiti Kebangsaan Malaysia (UKM) |
Disorders of gut- brain interaction (DGBIs), previously known as functional gastrointestinal disorders (FGIDs) are a group of conditions that cause long-term digestive symptoms such as:
- Stomach pain
- Nausea
- Bloating
- Constipation
- Diarrhoea
- A combination of the above issues, without any obvious structural or inflammatory disease
In Malaysia, the most common DGBIs are:
- Irritable bowel syndrome (IBS), a long-term condition that interferes with how your gut works, causing belly pain, bloating, gas, and sometimes diarrhea, sometimes constipation, or both.
- Functional dyspepsia (FD), a long-term stomach issue where you often feel uncomfortably full, bloated, or have a burning pain in your upper belly; however, the doctor can’t find anything wrong with your gastrointestinal tract.
| “Dyspepsia” is another word for indigestion. |
WHAT CAUSES GASTROINTESTINAL SYMPTOMS?
The exact causes of DGBI are not fully understood but people often experience symptoms due to:
Visceral Hypersensitivity
- People with DGBI are more sensitive to pain, their body reacting strongly even to normal gut functions or minor pain.
Motility Disturbances
- Motility refers to the gut’s ability to move food on its own through the small and large intestines, and out of the body.
- Diet, especially foods high in FODMAPs, can affect this by drawing water into the intestines, speeding up digestion, and causing symptoms like diarrhoea, nausea, and stomach pain.
FODMAPs
|
Altered Mucosal and Immune Function
- Eosinophil cells play a role in protecting the gut lining, maintaining its strength, and supporting immunity.
- Increased levels of these cells have been found in the colon of IBS patients, along with higher immune cell activity in the blood.
- In addition, the gut lining acts as a barrier to block harmful substances, but studies show the gut lining is often weaker in IBS patients.
Altered Gut Microbiota
- Gut bacteria can also speed up how fast food moves through the gut and creating conditions that favor certain bacteria.
- Studies found that IBS patients have different gut bacteria compared to healthy people, and this change leads to more fermentation, which causes symptoms.
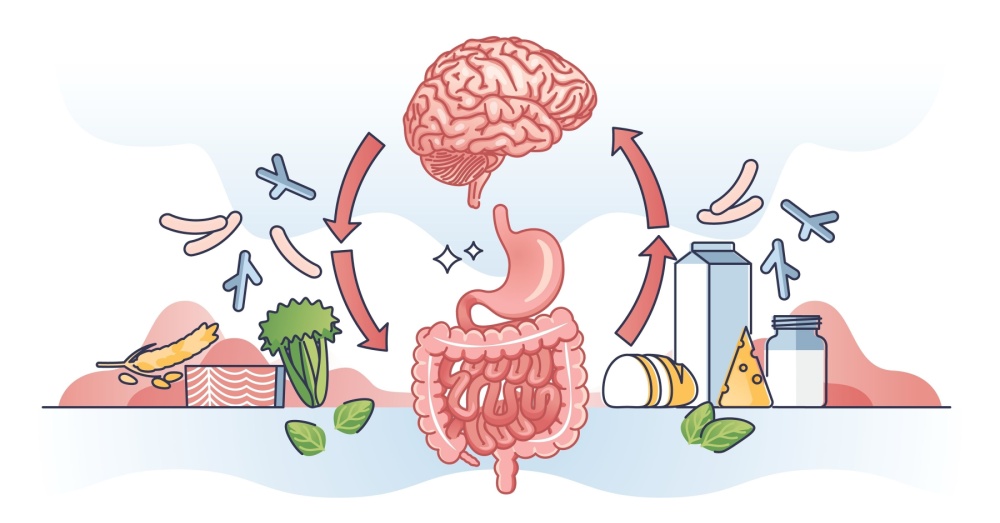
Altered Central Nervous System Processing
- Nerve sensitivity and an overactive immune system in DGBI can cause pain signals and weaken the gut lining, making it more prone to irritation.
- This overactivity also makes the gut more reactive to stress hormones, worsening symptoms. Magnetic resonance imaging (MRI) or brain scans studies of IBS patients have shown heightened activity in areas like the grey matter, which processes pain, and the insula, which is involved in emotions and awareness.
WHO ARE AT RISK?
- Individuals exposed to stress experience changes in the interaction between the brain and gut (gut-brain axis), which can ultimately trigger various gastrointestinal disorders.
- Individuals exposed to general trauma, as well as emotional, sexual, and physical abuse during childhood, can increase the risk of developing DGBI.
- Individuals who had taken antibiotics multiple times in the past, specifically, those who had three or more antibiotic prescriptions had about 3 to 4 6 times higher chance of being diagnosed with IBS, regardless of the type of antibiotic used. Antibiotics can indirectly alter the composition of the gut microbiota, and they are a risk factor for DGBI, particularly IBS.
- Individuals who have had gastroenteritis. Gastroenteritis is the irritation and inflammation of your stomach and intestines caused by viruses, bacteria, fungi, or parasites.
HOW DGBI IS MANAGED
Management of DGBI involves a variety of approaches with pharmacologic and brain-gut behavior therapies and specialist care as needed. The management also involves multidisciplinary team approaches such as physicians, gastroenterologists, dietitians and psychiatrists to help in patient management.
- Pharmacologic approaches, which involve using medications to treat symptoms like pain, bloating, and digestive issues.
- Diet therapies, with diets such as the Mediterranean diet or a low FODMAP diet to reduce symptoms.
- Brain-gut behavior therapies, which are treatments that focus on how stress and emotions affect digestion, using techniques like therapy or relaxation exercises to improve symptoms.
- Complementary or alternative therapies such as acupuncture may help manage symptoms by focusing on balancing the body’s energy and promoting overall wellness.
- Physical therapy, like pelvic floor therapy, may help people with digestive or abdominal issues. Those at risk include people with ongoing stomach problems, pelvic pain, or who have had surgery or childbirth.
DIETARY INTERVENTIONS FOR DGBI
Certain foods can trigger or worsen symptoms such as bloating, pain, or diarrhea, including:
- Fatty foods, dairy, high-fiber foods, spicy foods, and certain carbohydrates (like those found in beans, onions, or wheat) are broken down by gut bacteria.
- This breakdown produces gas and cause discomfort or flare-ups of symptoms.
#1 Eat Smaller, More Frequent Meals
- Instead of large meals, try eating 4 to 6 smaller meals throughout the day.
- This can help reduce bloating and discomfort.
#2 Avoid Trigger Foods
- Some foods may make symptoms worse. Common triggers include fatty foods, carbonated drinks, caffeine, alcohol, and spicy foods.
- Keep a food diary to help identify personal triggers like onions, garlic, mushrooms and others.
#3 Increase Your Fibre Intake
- Soluble fibre—commonly found in oats, beans, apples, and carrots—dissolves in water and helps with digestion.
- Insoluble fibre—found in (found in whole grains and some vegetables—adds bulk to stool and helps move food through the digestive system, which helps to address both diarrhea and constipation, common symptoms of DGBI.
| Some people living with DGBI find that following a low FODMAP diet, which reduces or eliminates certain carbohydrates that are poorly absorbed in the gut from their diet, can significantly help reduce symptoms. If you are interested in this diet, consult a dietitian for more information. |
#5 Stay Hydrated
- According to a study conducted in Australia, constipation affects up to 85% of people with DGBI.
- Drink 1.5 to 2 liters of water a day to help keep things moving smoothly through the gut, soften stools, and prevent constipation.
#6 Consider Probiotics
- Some studies suggest that probiotics can help balance the gut microbiome and improve symptoms.
- Consult a doctor and dietitian on how to incorporate probiotics into your diet.
This article is part of our series on tips and advice for leading a healthy lifestyle.
|