A Crick in the Neck
April 28, 2022 Return

Dr Eugene Wong Consultant Orthopaedic & Spine Surgeon
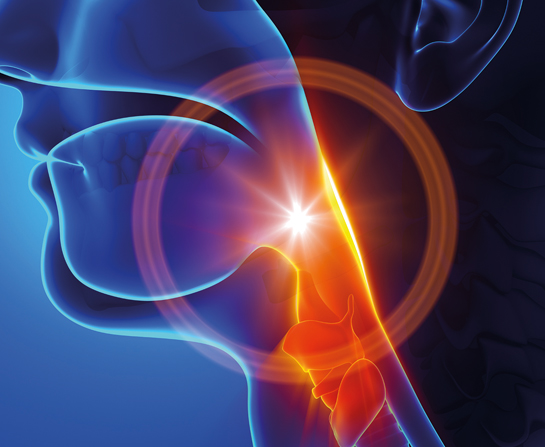
Neck pain is something that most of us have experienced before. It is that that feeling of pain and stiffness that can be either localized in the neck area or it may radiate down the arm and fingers. 10% of people have an episode of neck pain every year. Neck pain occurs more frequently in women than in men, and can be associated with stiffness, numbness or tingling, clicking sounds, dizziness, headaches, blackouts and muscle spasms.
1. What are the possible causes of neck pain?
Neck pain may be due to the following:
- Injury or degeneration affecting muscles or ligaments, soft-tissue strain
- Inflammation – rheumatoid arthritis, ankylosing spondylitis
- Infection – discitis, epidural abscess, meningitis
- Infiltration by tumours
Problems originating in areas other than the spine may also cause neck pain. These include cardiac pain, complex regional pain syndrome, entrapment syndromes, herpes zoster (shingles), spinal tumours, conditions affecting the rotator cuff (the tendons at the shoulder joint) and thoracic outlet syndrome (compression of the nerves and/or blood vessels between the collarbone and first rib).
2. What risk factors can contribute to acute neck pain?
Workplace environment can contribute to neck pain. For example, unhappiness and stress from the nature of one’s work or the social environment at the workplace. Also, involvement in a motor vehicle accident can contribute to the risk of neck pain in the future.
3. How do you diagnose the cause of neck pain?
First, we will need a detailed history, physical examination and the use of several diagnostic tests to find out the cause of your pain. Taking an X-ray of the neck is usually the first step and will help determine if more tests are needed. Magnetic resonance imaging (MRI) is commonly used to evaluate the spine because it can show abnormal areas of the soft tissues around the spine. MRI helps to find tumors, herniated discs, or other soft-tissue disorders.
The CT scan is most useful when a condition that only affects the bones of the spine is suspected. A bone scan is used to help locate the affected areas of the spine. Blood tests are done to look for infections or arthritis.
4. When should you seek treatment?
See a doctor when you have:
- Continuous and persistent pain.
- Severe intractable (incurable) or increasing pain.
- Radiating pain down the arms.
- Pain accompanied by headaches, numbness, tingling, or weakness.
- New symptoms before the age of 20 years or after 55 years.
- Weakness or loss of sensation along the spinal cord.
5. How is neck pain treated?
- In an acute injury, lie down on your back with a thin pillow or on your side with a thicker pillow to support the neck. This will relieve the pressure and relax any tight muscles. Ice will help decrease swelling and muscle spasms.
- Gently move your neck as soon as possible to regain full range of motion, reduce pain from swelling and muscle spasms, and prevent your muscles from becoming weak.
- Stretching exercises can help to relax the neck muscles and restore range of motion.
- Maintain proper postural alignment throughout the day in order to decrease any strain created on your neck.
- Diagnostic and therapeutic injections of local anesthetics and steroids.
- Surgery to remove the cause of pain and correct any other related medical conditions.
6. How do you take care of your neck?
- Maintain a good posture by holding your head up and keeping your shoulders back and down.
- Use the chair arm rests to support your arms when you are seated.
- Avoid sitting in the same position for prolonged periods of time. Take periodic breaks from the desk.
- Avoid looking up or down at a computer monitor. Adjust it to eye level.
- Avoid placing pressure over the upper back with backpacks, over-the-shoulder purses, or children riding on your shoulders.
- Do not perform overhead work for prolonged periods.
- Sleep with your neck in a neutral position by having a small pillow under the nape of your neck (sleeping on your back) or sleeping with enough pillows to keep your neck straight in line with your body (sleeping on your side).
- Carry heavy objects close to your body rather than with outstretched arms.
- Use relaxation methods when you feel stressed, tensed or worried, as these feelings can tighten your neck muscles and cause more pain.
- Stay at work or return to work as soon as possible even if the pain hasn’t completely gone.
- Think and stay positive – expect the neck pain to get better!
If you like this article, do subscribe here.