WORDS ASSOCIATE PROFESSOR DR KUMAR HARI RAJAH & ASSOCIATE PROFESSOR DR SOMANATHAN M N MENON
| FEATURED EXPERTS |
| ASSOCIATE PROFESSOR DR KUMAR HARI RAJAH School of Medicine Faculty of Health & Medical Sciences Taylor’s University |
| ASSOCIATE PROFESSOR DR SOMANATHAN M N MENON School of Medicine Faculty of Health & Medical Sciences Taylor’s University |
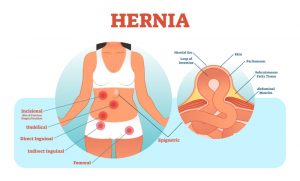
You may have heard of the term ‘hernia’ or ‘angin pasang’ once or twice before. Affecting both women and more commonly, men, many seek medical attention for reducible swellings which were discovered incidentally or swelling which suddenly appears during a period of physical straining.
WHAT IS HERNIA?
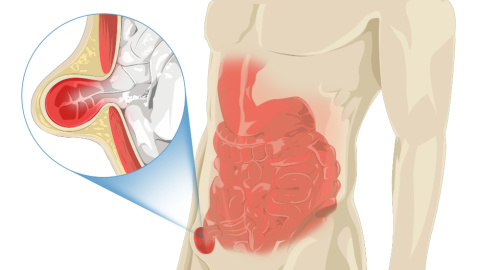
A hernia is defined as a protrusion, bulge, or projection of an organ or a part of an organ through the body wall that normally goes away on lying down.
They are extremely common and often seen in the groin.
Common risk factors
|
INGUINAL HERNIA
- The protrusion occurs through the inguinal canal in the body’s anterior abdominal wall.
- By far the most common medical conditions in which primary care physicians refer patients for surgery, comprising approximately 96 percent of all groin hernias.
- Generally, inguinal hernia affects all ages, but the incidence increases with regards to age.
- Women manifest inguinal hernia later with a median age of 60 to 79 years, unlike that of men which is 10 years earlier.
Inguinal hernias are traditionally classified as one of the following three types:
- Direct hernia. The hernia sac bulges directly through the posterior wall of the inguinal canal. It usually occurs in men over 40 years of age.
- Indirect hernia, which passes through the internal inguinal ring alongside the spermatic cord, following the coursing of the inguinal canal.
- Combined hernia. The hernia sacs are on both sides of the inferior epigastric vessels.
SIGNS THAT YOU MAY HAVE INGUINAL HERNIA
- A bulge in the area on either side of the pubic bone; there may be a burning, gurgling or aching sensation at the bulge.
- For male patients, pain and swelling can occasionally occur around the testicles, when the protruding intestine descends into the scrotum.
- Pain or discomfort in the groin, especially when bending over, coughing, or lifting.
DIAGNOSING INGUINAL HERNIA
Physical examination
Most early inguinal hernias can be diagnosed by careful physical examination.
The physical examination begins by carefully inspecting the inguinal areas for bulges while the patient is standing.
Then, the patient would be asked to cough or strain down (Valsalva manoeuvre) while the physician observes for bulges.
Imaging
Although imaging is rarely needed to diagnose a hernia, it may be useful in certain clinical situations such as suspected sports hernia, recurrent hernia, uncertain diagnosis, and surgical complications, (especially chronic pain).
Magnetic resonance imaging (MRI) provides the most sensitive detection of a hidden hernia in a patient with clinical suspicion for hernia.
TREATING INGUINAL HERNIA
There is currently no medical recommendation about how to manage an inguinal hernia condition.
Wait and see
Watchful waiting is a recommended reasonable option, especially for hernia with minimal symptoms.
Repair
Most inguinal hernia repairs can be performed safely, accurately, and cost-effectively using local anaesthesia, through an open anterior approach.
Hernia repair using prosthetic mesh would be a good choice in patients with a direct hernia or older patients with a longstanding hernia and attenuated fascia.
What about surgery?
Traditional hernia surgery carries a high risk of chronic pain, and as many as 17% of patients can have significant pain for years.
This high incidence is likely due to the location of the mesh used for this kind of surgery. It may also be related to nerve scarification, mesh contraction, chronic inflammation, or osteitis pubis.
Fortunately, there are procedures that lower this chronic pain, for example, the open pre-peritoneal repair, where the nerves responsible for the chronic pain are avoided, leading to a lower incidence of this problematic complication.
There are also minimally invasive surgical procedures involving transabdominal preperitoneal (TAPP) repair and total extraperitoneal repair (TEP). These procedures facilitate the placement of the mesh without any need for suturing, allowing passive pressure of the peritoneal contents to keep the mesh in place.
CAN WE PREVENT INGUINAL HERNIA FROM HAPPENING TO US?
Yes, you can reduce the risk of developing an inguinal hernia by reducing the pressure on the abdominal wall.
- Maintain a healthy weight. Extra weight will put more stress and pressure over the abdominal walls especially when one stands or moves.
- Be active and do the right exercises. Many exercises are available but doing the right exercises without overexertion is the key. Exercises like increasing core strength, sit ups, cycling and yoga are helpful.
- Avoid heavy lifting. Try not to lift objects if they are too heavy. If you must, adopt the right technique such as bending knees and lifting with your legs.
- Consume foods high in dietary fibre to reduce incidence of constipation; constipation can trigger a hernia when one strains during the passing of stools.
- Get treatment if you have urinary problems due to an enlarged prostate gland or if you have a chronic cough.
References:
- Onuigbo, W.I.B., & Nieze, G.E. (2016). Inguinal hernia. A review. Journal of surgery and operative care, 1(2). https://doi.org/10.15744/2455-7617.1.202
- Jenkins, J. T., & O’Dwyer, P. J. (2008). Inguinal hernias. BMJ (Clinical research ed.), 336(7638), 269–272. https://doi.org/10.1136/bmj.39450.428275.AD
- Öberg, S., Andresen, K., & Rosenberg, J. (2017). Etiology of inguinal hernias: A comprehensive review. Frontiers in surgery, 4, 52. https://doi.org/10.3389/fsurg.2017.00052
- Köckerling, F., & Simons, M. P. (2018). Current concepts of inguinal hernia repair. Visceral medicine, 34(2), 145–150. https://doi.org/10.1159/000487278