WORDS ASSOCIATE PROFESSOR DR KHINE PWINT PHYU, ASSOCIATE PROFESSOR DR GANESH RAMACHANDRAN & ASSOCIATE PROFESSOR DR ANITHA PONNUPILLAI
The International Day to End Obstetric Fistula, observed annually on 23 May, serves as a reminder of the silent suffering endured by women around the world.
 FEATURED EXPERT FEATURED EXPERTASSOCIATE PROFESSOR DR KHINE PWINT PHYU School of Medicine Faculty of Health and Medical Sciences Taylor’s University |
OBSTETRIC FISTULA EXPLAINED IN 5 KEY POINTS
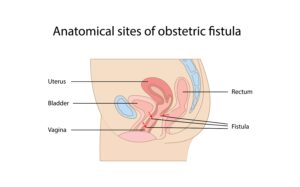
Click on the image for a larger, clearer version.
- Obstetric fistula is an excruciating childbirth injury resulting in an abnormal connection between a woman’s birth canal and bladder or rectum.
- The cause of obstetric fistulas lies in traumatic childbirth experiences. Prolonged and difficult labours subject women to prolonged pressure on the birth canal, resulting in inflammation, tissue damage, and death of cells.
- This can lead to the formation of fistulas, creating distressing symptoms such as urinary or faecal leakage, foul-smelling vaginal discharge, chronic vaginal infections, or painful sexual intercourse.
- Globally, 65% of obstetric fistula cases occur in girls under the age of 18, affecting impoverished and vulnerable girls and women.
- Despite its profound impact, obstetric fistula remains largely hidden in the shadows of societal taboos and healthcare disparities. However, empirically, because of the access most women in Malaysia have to good healthcare facilities, obstetric fistulas are exceedingly uncommon in our country.
 FEATURED EXPERT FEATURED EXPERTASSOCIATE PROFESSOR DR GANESH RAMACHANDRAN School of Medicine Faculty of Health and Medical Sciences Taylor’s University |
3 FACTORS THAT INCREASE THE RISK OF OBSTETRIC FISTULA
Limited Access to Skilled Healthcare
Inadequate access to skilled birth attendants and emergency obstetric care can lead to prolonged labour without proper medical intervention. This is the leading cause of severe birth trauma and fistula formation.
Poor Socioeconomic Conditions
Due to poverty and lack of education, young women in underprivileged environments can be subjected to childhood marriages, teenage pregnancies, and associated complications that include fistula formation.
Social Stigma and Cultural Barriers
Some cultural beliefs and societal stigma surrounding childbirth-related injuries impede timely medical interventions. Misconceptions and shame prevent women from seeking the necessary healthcare, thus exacerbating the severity of obstetric fistulas.
 FEATURED EXPERT FEATURED EXPERTASSOCIATE PROFESSOR DR ANITHA PONNUPILLAI School of Medicine Faculty of Health and Medical Sciences Taylor’s University |
INITIATIVES THAT MUST BE TAKEN TO REDUCE THE INCIDENCE OF OBSTETRIC FISTULAS
Promote Access to Quality Maternal Healthcare
- Strengthen maternal healthcare services, especially in remote areas, is crucial.
- Ensure healthcare for all, with emphasis on accessible care during pregnancy, labour, and after childbirth.
Health Education Initiatives
- Public awareness campaigns and access to education are instrumental in dispelling myths and fostering early recognition of birth injuries.
- Empower women with knowledge about childbirth complications.
- Encourage proactive seeking of medical assistance and reduces the stigma surrounding fistulas.
Enhance Healthcare Infrastructure
- Invest in healthcare infrastructure, including skilled birth attendants, surgical facilities, and postoperative rehabilitation services, play a crucial role.
- Provide adequate resources and training for healthcare professionals to assist in ensuring timely diagnosis, treatment, and rehabilitation of obstetric fistula patients.
Conduct Population Studies and Research
- Conduct comprehensive population studies on the prevalence and incidence of obstetric fistula to establish accurate regional data.
- Use the data from these studies to dentify causative factors to shed light on the root causes and also to curtail and eliminate the factors responsible for obstetric fistulas.
WHAT ARE WE DOING IN MALAYSIA TO ADDRESS THE PROBLEM?
In Malaysia, extensive measures are taken to ensure that both urban and rural areas receive adequate care during pregnancy, labour, and childbirth.
Intensive training programs for midwives are conducted to ensure the delivery of babies with safe techniques and the timely diagnosis of serious postpartum complications, including obstetric fistulas.
Furthermore, urogynaecology departments have been established in both private and public sectors, staffed with trained urogynaecologists to effectively treat obstetric fistulas efficiently if at all they occur and provide comprehensive rehabilitation services.